Pancreatic cancer has long maintained a daunting reputation as one of the most aggressive and difficult-to-treat malignancies, a challenge largely defined by its resistance to standardized therapies and the limitations of conventional research models. For patients and clinicians alike, the path of treatment has often been a frustrating process of trial and error, with outcomes that have barely shifted in decades. Now, a groundbreaking development in biotechnology is poised to rewrite this narrative entirely by bringing the fight against cancer to a deeply personal level. By growing miniature, living replicas of a patient’s own tumor in the laboratory, researchers are unlocking the ability to test and predict treatment efficacy with unprecedented accuracy, heralding a new era where therapy is not just prescribed, but precisely engineered for the individual. This approach promises to transform clinical decision-making from an educated guess into a data-driven science, offering a tangible beacon of hope against a notoriously challenging disease.
A New Frontier in Cancer Modeling
The advent of patient-derived organoids represents a fundamental shift in how cancer is studied outside the human body. These sophisticated, three-dimensional cellular structures are cultivated from a patient’s own cancer stem cells, meticulously grown in a laboratory setting to mimic the complex architecture, cellular diversity, and physiological function of the original tumor. Unlike traditional two-dimensional cell cultures, which are grown as a flat layer on a plastic dish and fail to capture the intricate interplay between different cell types, organoids successfully recreate the tumor microenvironment. This high-fidelity replication provides a significantly more accurate and clinically relevant platform for investigating tumor biology, understanding individual patient variations, and assessing therapeutic responses. The ability to model the disease with such precision is not merely an incremental improvement but a revolutionary leap forward, offering profound insights that were previously unattainable with older, less representative experimental systems.
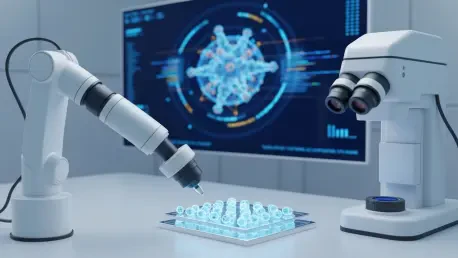
At the core of this innovative approach is a rigorous and meticulous methodology for generating these living tumor avatars. The process begins with the careful isolation of cancer cells from a small tissue sample obtained during a surgical procedure or biopsy. These cells are then placed in a specialized gel matrix and nourished with a unique cocktail of growth factors, creating laboratory conditions that closely replicate the natural, or in vivo, environment of the pancreas. This painstaking attention to detail is paramount, as it ensures the resulting organoids retain the crucial genetic mutations and phenotypic characteristics of the patient’s tumor from which they were derived. By successfully creating these intricate, patient-specific biological replicas, researchers have developed a powerful and dynamic tool. Each organoid culture serves as a personal surrogate for a patient’s cancer, allowing for a wide range of experiments to be conducted ex vivo that can reliably predict how the actual tumor will behave in vivo.
Revolutionizing Treatment Selection and Strategy
One of the most immediate and impactful applications of patient-derived organoids is their use in comprehensive and predictive drug screening. Scientists can establish an array of these mini-tumors and expose them to a broad panel of therapeutic agents, ranging from established chemotherapies used in current clinical practice to novel, investigational drugs still in development. This allows for a multifaceted approach to personalizing therapy. First, it enables the pre-treatment identification of the most potent drugs for an individual’s specific tumor, effectively eliminating the trial-and-error process that often subjects patients to the debilitating side effects of toxic and ineffective treatments. The resulting “organoid drug-sensitivity profile” provides oncologists with a clear, evidence-based roadmap for selecting the most promising therapeutic regimen from the very beginning. This targeted strategy not only maximizes the potential for a positive response but also spares patients from unnecessary physical and emotional hardship.
Beyond identifying the most effective initial treatment, this technology provides a unique window into one of cancer’s greatest challenges: the development of drug resistance. By continuously treating the organoids over time, researchers can observe how the cancer cells adapt and evolve to evade the effects of a particular therapy. This allows them to study the underlying biological mechanisms that drive resistance, a critical step in developing strategies to overcome it. This foresight is invaluable in a clinical setting. By understanding how a patient’s tumor might eventually stop responding to a given treatment, clinicians can anticipate this challenge and develop proactive management plans. For instance, they could prepare to switch to a different therapy at the first sign of resistance or introduce a combination of drugs designed to preemptively block escape pathways, thereby staying one step ahead of the disease’s progression and extending the duration of effective treatment.
The Synergy of Genomics and Living Models
The true power of this platform is fully realized when organoid biology is integrated with advanced genomic sequencing techniques. This potent combination facilitates a deep and comprehensive investigation into the molecular underpinnings of an individual’s pancreatic cancer, moving far beyond what can be observed by drug responses alone. High-throughput sequencing of the organoid DNA and RNA reveals the complete catalog of genetic alterations, specific mutations, and gene expression profiles that are driving the tumor’s relentless growth and survival. This process creates a detailed molecular blueprint that is unique to each patient’s disease. Armed with this information, clinicians can understand precisely which cellular pathways have been hijacked by the cancer, providing a clear map of its vulnerabilities. This level of insight transforms the tumor from an enigmatic adversary into a well-defined target with identifiable weaknesses that can be exploited therapeutically.
This detailed molecular blueprint is the very essence of precision medicine, an approach that abandons the traditional, one-size-fits-all model in favor of treatments tailored to an individual’s unique biological makeup. By correlating the genetic data with the drug sensitivity results from the organoid screening, oncologists can make highly informed decisions. For example, if sequencing reveals a specific mutation in a growth-signaling pathway, they can select a targeted therapy specifically designed to inhibit that pathway. This ability to match a treatment directly to a tumor’s molecular profile holds the potential to dramatically improve clinical outcomes while minimizing collateral damage to healthy cells. It represents a paradigm shift from treating “pancreatic cancer” as a single disease to treating the specific molecular variant of the disease present in each patient, ensuring that every individual receives the therapy most likely to be effective for them.
Forging a Path to Adaptive Therapy
A significant and persistent hurdle in oncology has been the “translational gap”—the profound disconnect between promising discoveries made in the laboratory and their successful application in real-world clinical settings. The framework established through this research served as a vital and practical bridge across this gap. The work laid the foundation for a future clinical reality where organoid-based testing could become a standard component of a patient’s initial diagnostic workup. In this model, an oncologist would send a tumor sample for organoid cultivation and analysis, and in a matter of weeks, receive a comprehensive report. This report would detail the tumor’s molecular profile and its sensitivity to a panel of drugs, providing empirical, patient-specific data to guide treatment decisions. This approach transformed the process of selecting a therapy from a generalized protocol into a personalized, evidence-based strategy, paving a tangible pathway for translating fundamental research insights directly into improved patient care.
The vision established by this research ultimately pointed toward a future of dynamic and adaptive cancer management. It became clear that generating organoid models at various intervals throughout a patient’s treatment journey—such as after a course of chemotherapy or upon evidence of disease progression—offered a powerful method for tracking the tumor’s biological evolution in real time. This dynamic monitoring allowed clinicians to continuously adapt treatment plans in response to emerging changes in drug sensitivity or the development of new resistance mechanisms. Such an approach represented a truly personalized and adaptive strategy for cancer care, one that could significantly extend and improve patients’ lives. The necessary interdisciplinary collaboration among oncologists, molecular biologists, and bioinformaticians, fostered by this foundational work, was essential in refining the technology and establishing the standardized protocols that made this visionary application a clinical possibility.