Recurrent pregnancy loss, often referred to as RPL and characterized by two or more consecutive miscarriages, casts a heavy shadow over the dreams of countless couples hoping to build a family. For those navigating the complex world of in vitro fertilization (IVF), a beacon of hope emerges through Preimplantation Genetic Testing for Aneuploidy (PGT-A), a method designed to identify chromosomally normal embryos for transfer. A recent 7-year retrospective cohort study published in Reproductive Sciences has delved into a pressing question: what is the ideal number of blastocysts—early-stage embryos—to test via PGT-A to enhance success rates for RPL patients? This research not only offers evidence-based insights but also promises to redefine clinical strategies in reproductive medicine. By addressing both the scientific and human elements of fertility challenges, the findings pave the way for more informed decisions, balancing the pursuit of pregnancy with the emotional and financial realities faced by patients on this journey.
The Science Behind PGT-A for RPL Patients
Understanding Chromosomal Abnormalities
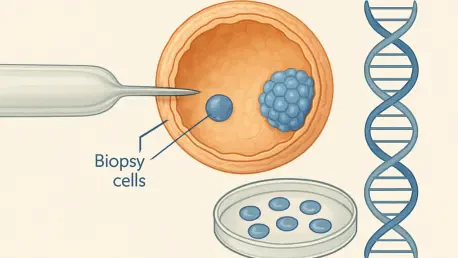
The significance of PGT-A in managing recurrent pregnancy loss lies in its ability to screen embryos for chromosomal abnormalities, which are widely recognized as a primary cause of miscarriage in RPL cases. Many couples experience repeated heartbreak due to aneuploidy, where embryos carry an incorrect number of chromosomes, leading to failed implantations or early pregnancy loss. The technology behind PGT-A allows clinicians to analyze blastocysts before transfer, ensuring that only those with a normal chromosomal profile are selected. This targeted approach has shown promise in reducing miscarriage rates and boosting the chances of a viable pregnancy. As the study by Liao et al. indicates, identifying euploid embryos is a game-changer for patients who have endured multiple losses, offering a scientifically grounded path forward in their fertility journey while addressing one of the root causes of their struggles.
Beyond the basic mechanics of genetic screening, the broader implications of PGT-A reveal its transformative potential within assisted reproductive technologies. Chromosomal issues are not just numbers on a lab report; they represent the silent barriers that prevent many pregnancies from progressing. The research highlights how testing blastocysts through PGT-A can significantly shift outcomes by prioritizing embryos most likely to result in a healthy birth. Importantly, this method does not guarantee success in every case, but it substantially narrows down the risks for RPL patients. The study also points to the need for precise diagnostic tools to ensure accurate results, as misidentification could lead to the transfer of non-viable embryos or the discarding of potentially healthy ones. This underscores a critical intersection of technology and clinical expertise in modern fertility care.
Importance of Blastocyst Quality
A pivotal factor in the success of PGT-A for RPL patients is the quality of the blastocysts being tested, as not all embryos are equally suited for genetic analysis or implantation. High-quality blastocysts, assessed through morphological criteria such as cell symmetry and developmental stage, are far more likely to yield reliable genetic results and achieve successful pregnancy outcomes. The research emphasizes that poor-quality embryos often fail to provide conclusive data or survive the transfer process, rendering testing efforts futile. This insight shifts the focus from merely increasing the number of embryos tested to ensuring that only those meeting strict quality standards are considered, thereby optimizing both clinical resources and patient expectations in the challenging landscape of IVF.
Moreover, the emphasis on blastocyst quality introduces a nuanced layer to fertility treatment protocols for those with recurrent losses. Clinicians must balance the urge to test as many embryos as possible with the reality that substandard blastocysts may not contribute to a positive result, regardless of genetic normalcy. This perspective encourages a more selective approach during IVF cycles, where embryologists play a crucial role in grading and prioritizing embryos before PGT-A is even applied. Such meticulous evaluation helps mitigate the risk of wasted cycles and emotional disappointment for patients already burdened by repeated setbacks. The study advocates for refined laboratory practices to enhance embryo assessment, ensuring that quality remains a cornerstone of effective genetic testing strategies.
Factors Influencing Blastocyst Count
Patient-Specific Variables
When determining the optimal number of blastocysts to test via PGT-A for RPL patients, individual factors such as maternal age emerge as critical considerations that can dramatically influence outcomes. Younger patients often exhibit lower rates of chromosomal abnormalities in their embryos, meaning fewer blastocysts may need to be tested to identify a viable candidate for transfer. In contrast, older patients face a higher likelihood of aneuploidy, often necessitating a larger pool of embryos to increase the odds of finding a chromosomally normal one. The research by Liao et al. underscores that tailoring the testing strategy to these personal variables can make a significant difference in achieving a successful pregnancy while avoiding unnecessary interventions that might prolong the treatment process.
Additionally, other patient-specific elements, such as the history of prior pregnancy losses and overall reproductive health, play a vital role in shaping the approach to PGT-A testing. For instance, a patient with multiple unexplained miscarriages might require a more extensive evaluation of blastocysts to uncover underlying genetic issues, while someone with a known cause of loss might benefit from a more focused strategy. The study highlights the importance of comprehensive pre-treatment assessments to guide clinical decisions, ensuring that the number of embryos tested aligns with the unique medical profile of each individual. This personalized framework not only enhances the efficiency of IVF cycles but also respects the diverse needs and circumstances of those grappling with recurrent pregnancy loss.
Emotional and Ethical Considerations
The journey of fertility treatment for RPL patients extends far beyond clinical procedures, delving into profound emotional and ethical territories that accompany PGT-A and embryo selection. The repeated cycles of hope and disappointment can take a severe psychological toll, with many couples grappling with stress, anxiety, and grief as they navigate IVF. The decision to test multiple blastocysts often intensifies these feelings, as each round of testing carries the weight of potential success or another setback. The research advocates for integrating mental health support into treatment plans, recognizing that emotional resilience is just as crucial as medical intervention in helping patients endure the uncertainties of this path.
Equally complex are the ethical dilemmas surrounding the selection and potential discarding of embryos based on PGT-A results, which can raise deep moral questions for many individuals. Some couples may struggle with the idea of prioritizing certain embryos over others, while others might face societal or personal conflicts regarding the fate of non-viable embryos. The study by Liao et al. stresses the importance of counseling to address these concerns, ensuring that patients are fully informed about the implications of their choices. By fostering open discussions between clinicians, genetic counselors, and patients, fertility care can better navigate these sensitive issues, aligning medical decisions with personal values and emotional well-being in the context of recurrent pregnancy loss.
Balancing Benefits and Burdens
Financial and Practical Challenges
One of the most pressing hurdles in utilizing PGT-A for RPL patients is the financial burden associated with testing multiple blastocysts, often compounded by the high costs of repeated IVF cycles. Each round of testing and treatment can add significant expenses, placing a strain on couples already navigating the emotional challenges of recurrent loss. The research suggests that beyond a certain threshold, additional testing may yield diminishing returns, meaning the likelihood of identifying a viable embryo does not proportionally increase with the number of blastocysts analyzed. This finding urges both clinicians and patients to carefully evaluate the cost-benefit ratio, ensuring that resources are allocated effectively without subjecting individuals to unnecessary financial hardship.
Furthermore, the practical challenges of undergoing multiple IVF cycles to obtain enough blastocysts for PGT-A cannot be understated, as the process often involves time-intensive procedures and physical demands on the body. For many, the logistics of frequent clinic visits, hormone treatments, and recovery periods add layers of complexity to an already arduous journey. The study highlights the need for transparent communication about the realistic outcomes of extensive testing, helping patients set achievable goals while managing expectations. By focusing on strategic planning—such as banking embryos over fewer, well-timed cycles—fertility clinics can help mitigate some of these practical barriers, making the process more sustainable for those pursuing treatment amidst recurrent pregnancy loss.
Personalized Treatment Approaches
The push for personalized treatment plans in reproductive medicine has gained momentum, particularly in the context of PGT-A for RPL patients, where a one-size-fits-all model falls short of addressing individual needs. The research by Liao et al. emphasizes that the optimal number of blastocysts to test must be determined through a detailed evaluation of each patient’s medical history, genetic profile, and personal circumstances. This tailored approach ensures that testing strategies are neither overly aggressive, risking unnecessary strain, nor too conservative, potentially missing viable embryos. Tailoring care in this manner fosters a sense of agency for patients, allowing them to feel more involved in decisions that profoundly impact their future.
Moreover, customization extends to the integration of supportive measures alongside clinical interventions, recognizing that fertility treatment is not solely a medical endeavor but a deeply human experience. For instance, adjusting the pace of IVF cycles or the extent of PGT-A testing based on a patient’s emotional readiness can significantly improve their overall well-being during treatment. The study advocates for collaborative decision-making, where reproductive endocrinologists work closely with patients to craft plans that reflect both scientific evidence and personal priorities. This shift toward individualized care not only enhances clinical outcomes but also builds trust, ensuring that those facing recurrent pregnancy loss receive compassionate, effective support tailored to their unique journey.
Future Directions in Reproductive Medicine
Evolving Technologies and Research
The landscape of reproductive medicine is undergoing rapid transformation, driven by advancements in genetic testing technologies that continue to refine the application of PGT-A for RPL patients. Innovations in sequencing methods and diagnostic accuracy are enhancing the ability to detect chromosomal abnormalities with greater precision, potentially reducing the number of blastocysts needed for testing in the future. The study by Liao et al. underscores the importance of ongoing research to validate these emerging tools, ensuring they translate into tangible benefits for couples seeking successful pregnancies. Staying abreast of such developments is critical for clinicians aiming to offer cutting-edge care in a field where every breakthrough could mean the difference between heartbreak and hope.
Equally vital is the commitment to expanding the body of evidence through long-term studies that track the outcomes of PGT-A across diverse patient populations. Current research, while promising, often focuses on specific demographics, leaving gaps in understanding how factors like ethnicity or socioeconomic status might influence results. The findings encourage investment in comprehensive data collection over the coming years, fostering a deeper grasp of how to optimize blastocyst testing protocols. This forward-looking approach ensures that reproductive medicine evolves in step with technological progress, continuously improving the prospects for those battling recurrent pregnancy loss through informed, evidence-based practices.
Multidisciplinary Care as a Cornerstone
A defining trend in modern fertility treatment for RPL patients is the growing recognition of multidisciplinary care as an essential component of successful outcomes, extending support beyond the confines of medical procedures. The integration of genetic counselors, mental health professionals, and reproductive endocrinologists creates a holistic framework that addresses the complex needs of couples undergoing PGT-A. The research highlights that counseling on genetic risks and emotional challenges can empower patients to make informed decisions about blastocyst testing, while also providing a safe space to process the grief and stress tied to recurrent loss. This collaborative model enhances the overall treatment experience by prioritizing well-being alongside clinical goals.
Additionally, multidisciplinary care serves as a bridge between cutting-edge science and the human side of fertility struggles, ensuring that patients are not reduced to mere data points in a lab. For instance, mental health support can help individuals cope with the uncertainty of waiting for PGT-A results, while genetic counseling clarifies the implications of test outcomes for future family planning. The study advocates for fertility clinics to establish robust networks of specialists who work in tandem to guide patients through every stage of their journey. By embedding this comprehensive approach into standard practice, the field can better serve those facing recurrent pregnancy loss, offering not just medical solutions but a compassionate partnership in their pursuit of parenthood.