Prostate cancer remains one of the most common cancers among men, and while hormone therapies have significantly improved patient outcomes, resistance to these treatments is a major challenge. The emergence of NXP800, a novel drug currently under clinical trials, offers a promising new approach to treating hormone-resistant prostate cancer.
The Challenge of Hormone Therapy Resistance
Limitations of Current Hormone Therapies
Hormone therapies such as enzalutamide and abiraterone have been game-changers in the treatment of advanced prostate cancer. These drugs work by inhibiting the androgen receptor pathway, which is crucial for the growth and survival of prostate cancer cells. Over time, many patients develop resistance to these treatments, rendering them ineffective. This resistance poses a significant hurdle, as it limits the long-term efficacy of hormone therapies and leaves patients with fewer treatment options. The development of resistance to these therapies underscores the urgent need for new treatment strategies to combat this pervasive issue.
Hormone-resistant prostate cancer presents a critical challenge in medical oncology. The emergence of resistance to otherwise life-saving treatments creates an urgent need for innovative solutions. Initial successes seen with enzalutamide and abiraterone, by targeting the androgen receptor pathway, marked significant advances. Nonetheless, the development of resistance has necessitated the search for different approaches. Consequently, researchers have been exploring various avenues to overcome this resistance, including targeting different molecular pathways involved in cancer progression. NXP800 represents one such innovative approach, offering hope and potential alternatives for patients who have exhausted existing therapeutic options.
The Need for New Treatment Options
As hormone therapies’ long-term effectiveness diminishes due to resistance, the biochemical landscape of prostate cancer treatment calls for novel solutions. Current research trends emphasize the importance of diverse treatment strategies to address the growing challenge of resistance. This necessity has propelled the scientific community to tirelessly seek solutions targeting alternative pathways crucial to cancer cell survival and proliferation. One such promising contender in this scientific quest is NXP800, designed to outmaneuver the traditional vulnerability points exploited by prostate cancer cells to evade existing therapies.
The development of NXP800 introduces a fresh perspective into the treatment paradigm of hormone-resistant prostate cancer. It operates on an innovative front, targeting pathways hitherto left underexploited in therapeutic designs. By honing in on specific molecular mechanisms, NXP800 could potentially bridge the gap left by conventional therapies’ waning effectiveness. Moreover, this new avenue opens possibilities for personalized medicine approaches, where treatments can be fine-tuned based on individual patient genetic profiles, enhancing overall efficacy.
NXP800: A Novel Mechanism of Action
Targeting the HSF1 Pathway
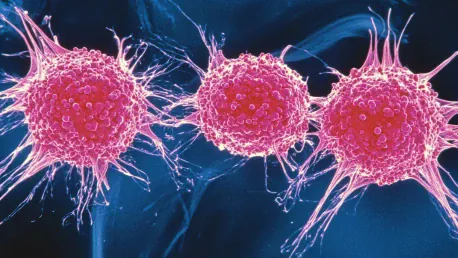
NXP800 operates through a unique mechanism by targeting the Heat Shock Factor 1 (HSF1) pathway. HSF1 acts as a master regulator in cells, controlling the production of heat shock proteins that help cancer cells survive under stressful conditions. By inhibiting this pathway, NXP800 disrupts the protective mechanisms of cancer cells, making them more vulnerable to treatment. The HSF1 pathway has long been recognized for its role in the cellular stress response, which cancer cells exploit to thrive even in hostile environments. By destabilizing the cellular defenses facilitated by HSF1, NXP800 potentially leaves cancer cells exposed to both internal and external stressors, thereby enhancing their susceptibility to treatment interventions.
This mechanistic approach places emphasis on dismantling the cellular foundation that supports cancer cell survival. Traditional therapies have largely focused on more apparent targets, often leaving these underlying mechanisms intact, inadvertently allowing cancer cells to recuperate and thrive. What sets NXP800 apart is its strategic target, aiming not just to attack cancer cells directly but to weaken their inherent resistance capabilities, thus making them more amenable to destruction by therapeutic measures. This innovative approach marks a significant shift in treating cancer, targeting the very survival toolkit of the malignant cells.
The Role of Heat Shock Proteins in Cancer
Heat shock proteins (HSPs) play a critical role in cancer progression by aiding in the proper folding and functioning of other proteins within the cell. Elevated levels of these proteins are often associated with more aggressive cancer and poorer patient outcomes. In prostate cancer, high levels of heat shock proteins have been linked to shorter survival times, highlighting the potential impact of targeting this pathway. Research has shown that heat shock proteins act as molecular chaperones, stabilizing unfolded or misfolded proteins and preventing cellular stress, thus contributing to tumor growth and resistance to therapy. Targeting these proteins could, therefore, disrupt the intricate balance within cancer cells, pushing them toward cellular breakdown and death.
The significance of this approach is further underscored by the correlation between heat shock protein levels and patient prognosis. Patients with high levels of these proteins tend to have a more aggressive disease course and shorter survival periods. This correlation amplifies the potential impact of a drug like NXP800, which aims to inhibit the production of heat shock proteins by blocking the HSF1 pathway. Such a strategy could tilt the balance toward improved survival outcomes by undermining a key survival mechanism of the cancer cells. The promise lies not just in halting cancer progression but in fundamentally altering the cellular environment to favor therapeutic success.
Preclinical Evidence of Efficacy
Laboratory Studies
In laboratory settings, NXP800 has shown significant promise in inhibiting the growth of prostate cancer cells. Researchers have conducted extensive studies on cell lines, demonstrating that the drug effectively reduces the proliferation of cancer cells, including those resistant to enzalutamide. These findings provide a strong foundation for further investigation in clinical trials. Laboratory studies have employed robust methodologies to assess the tumor-inhibiting potential of NXP800, utilizing various prostate cancer cell lines. The reproducibility of results across different experimental setups underscores the consistency and reliability of the observed effects, bolstering confidence in moving these studies to the clinical trial phase.
Details from these laboratory explorations reveal the intricate workings of NXP800. By focusing on its effects on cancer cell proliferation at the cellular level, researchers can map out the drug’s efficacy accurately. The consistent observation of growth inhibition, even in enzalutamide-resistant cells, highlights the potential of NXP800 as a versatile treatment option against hormone-resistant prostate cancer. Moreover, these data form the scientific backbone for designing future clinical trials, guiding dosage considerations, and highlighting potential biomarkers for therapy monitoring.
Animal Model Results
Animal models have played an instrumental role in evaluating the efficacy of NXP800. In mouse models of prostate cancer, the drug has been shown to significantly delay tumor growth compared to untreated controls. These preclinical results are encouraging, suggesting that NXP800 could offer a new therapeutic option for patients with advanced prostate cancer. The use of animal models provides a more complex biological environment, allowing researchers to assess the drug’s performance in a living organism. These models mimic human disease progression, providing invaluable insights into the potential clinical benefits and limitations of NXP800.
The promising results observed in animal studies bolster the ongoing translation of NXP800 from laboratory settings to human trials. Delays in tumor growth and reductions in tumor proliferation rates in these models align well with the desired therapeutic outcomes for advanced prostate cancer. These findings pave the way for clinical hypotheses and refined therapeutic strategies. By mimicking human pathophysiology in a controlled environment, animal studies establish a preliminary understanding of drug dynamics, efficacy, and safety profiles, crucial steps before initiating comprehensive human trials.
Clinical Trial Prospects
The recent advancements in biomedical research have sparked significant interest in the potential of new clinical trials. Scientists are hopeful that these trials will lead to groundbreaking treatments for a range of diseases, offering new hope to patients worldwide. As these trials progress, careful monitoring and stringent regulatory oversight will be crucial to ensure the safety and efficacy of new therapies. The outcomes of these trials could potentially revolutionize the medical field and provide much-needed solutions to currently incurable conditions.
Current Clinical Trials
NXP800 is currently undergoing clinical trials for ovarian and bile duct cancer, with promising preliminary results. These trials are crucial for establishing the safety and efficacy of the drug in humans. The success of these trials will pave the way for future studies specifically targeting prostate cancer. Clinical trials are essential in transitioning from the promising preclinical data to validated human clinical applications. They provide the necessary framework for assessing the therapeutic potential of NXP800 in actual patient populations, adhering to rigorous scientific and ethical standards.
The progress in ongoing trials offers hope for a potential extension of NXP800 applications. Preliminary human trial results indicating safety and efficacy in related cancer types enhance the credibility of pursuing dedicated prostate cancer trials. Each trial phase focuses on critical milestones, from initial safety assessments in Phase I to rigorous efficacy evaluations in later phases. Successfully navigating these trials builds a comprehensive understanding of the drug’s real-world applicability, directing future therapeutic pathways and integration into clinical practice.
Fast-Track and Orphan Drug Designation
The U.S. Food and Drug Administration (FDA) has granted NXP800 Fast-Track and Orphan Drug Designation for its application in ovarian, fallopian tube, peritoneal, and bile duct cancers. These designations facilitate a quicker review process and provide economic incentives, highlighting the potential impact of NXP800 in treating rare and hard-to-treat cancers. Fast-Track designation accelerates the drug development and approval process, ensuring that promising treatments reach patients sooner. Orphan Drug designation provides further incentives, such as tax credits for clinical trial costs, reduced regulatory fees, and market exclusivity upon approval.
These FDA designations reflect the promising potential and urgent need for innovative treatments like NXP800 in oncology. The regulatory support underscores the significance of NXP800’s mechanism and therapeutic promise across multiple cancer types. For patients and healthcare providers, this means expedited access to potentially lifesaving treatments. For the research community, it signifies recognition of the scientific advancements embodied in NXP800. These designations not only streamline the path to market availability but also provide a framework for robust clinical validation and future research endeavors.
Implications for Prostate Cancer Treatment
The attention given to prostate cancer treatment has increased significantly over the years, reflecting advancements in both medical research and clinical applications. Innovations in diagnostic techniques and targeted therapies promise improved outcomes for patients, marking a critical shift in the management of this prevalent disease. Moreover, the development of personalized medicine allows for tailored treatment plans, addressing the unique genetic and biological characteristics of each patient’s cancer. The integration of these cutting-edge strategies is helping to pave the way for more effective and less invasive treatment options, ultimately aiming to enhance the quality of life for those affected by prostate cancer.
Potential Impact on Patient Survival
If NXP800 proves effective in clinical trials, it could significantly impact patient survival rates. By offering a new treatment option for hormone-resistant prostate cancer, the drug has the potential to extend the lives of patients who have limited alternatives. This could represent a major advancement in the management of advanced prostate cancer. Improved survival outcomes would translate into a substantial shift in the therapeutic landscape, offering new hope to patients and their families. Additionally, extending survival while maintaining or improving quality of life would address critical unmet needs in prostate cancer care.
The potential impact on patient survival highlights the broader ramifications of successfully integrating NXP800 into clinical practice. For patients battling advanced stages of prostate cancer with limited effective treatments, NXP800 could serve as a beacon of hope. The drug’s novel mechanism and preliminary efficacy lend credence to the possibility of improved overall survival and progression-free survival outcomes. Such advancements could redefine standard care protocols, incorporating NXP800 as a cornerstone in the therapeutic regimen for hormone-resistant prostate cancer.
Identifying Suitable Patient Groups
Understanding the mechanism of NXP800 and its effects on the HSF1 pathway can help identify which patient groups are most likely to benefit from the treatment. Personalized medicine approaches, which tailor treatments based on individual patient characteristics, could enhance the efficacy of NXP800 and improve patient outcomes. Identifying specific biomarkers associated with HSF1 pathway activity could guide the selection of patients who would respond best to this targeted approach. This precision medicine strategy aligns with the broader trend in oncology to develop personalized treatment plans that maximize therapeutic benefits while minimizing side effects.
By honing in on suitable patient groups, the clinical application of NXP800 can be optimized to yield the highest efficacy. Biomarker-driven trials and genetic profiling can identify patients whose tumors exhibit high dependency on the heat shock response pathway. Such targeted interventions not only improve efficacy but also reduce unnecessary exposure to potentially ineffective treatments. Personalized treatment plans derived from robust biomarker studies would embody a sophisticated, patient-centered approach, potentially setting new standards in the therapeutic management of hormone-resistant prostate cancer.
Future Directions in Research
Expanding Clinical Trials
The next critical step for NXP800 is to expand clinical trials to include prostate cancer patients. These trials will be essential in validating the drug’s efficacy and safety in this specific patient population. Successful trials could lead to regulatory approval and widespread clinical use of NXP800 in treating hormone-resistant prostate cancer. Expanding clinical trials involves meticulous design and collaboration across research institutions and healthcare providers. This expansion is essential to gather comprehensive data on NXP800’s performance in diverse patient demographics and clinical settings.
Strategically expanding trials ensures thorough evaluation and generates the robust evidence required for regulatory submissions. This entails planning multi-phase studies, starting from pilot trials to larger, randomized controlled trials. Collaboration with key oncology centers and involving a diverse patient population will enable an accurate assessment of NXP800’s true clinical potential. Successful trial outcomes would lay the foundation for integrating NXP800 into clinical practice, offering a validated and approved treatment option for those with hormone-resistant prostate cancer.
Exploring Combination Therapies
Researchers are also exploring the potential of combining NXP800 with other treatments to enhance its efficacy. Combination therapies, which use multiple drugs to target different pathways simultaneously, could offer a more comprehensive approach to overcoming drug resistance and improving patient outcomes. Combining NXP800 with existing hormone therapies or other molecular inhibitors could synergistically enhance therapeutic effectiveness. Such strategies are particularly relevant in cases of advanced prostate cancer, where multifaceted treatment approaches may be necessary to achieve optimal results.
The exploration of combination therapies represents a forward-thinking approach in cancer treatment. By leveraging the complementary mechanisms of different drugs, combination therapies aim to maximize therapeutic efficacy and minimize resistance. Preclinical studies and early-phase clinical trials are vital in identifying the most promising combinations and understanding the interplay between different treatments. This approach holds the potential not only to improve response rates but also to set new benchmarks in the treatment of hormone-resistant prostate cancer, resulting in longer, healthier lives for patients.
Conclusion
Prostate cancer remains a significant health concern for men, being one of the most common types of cancer affecting this population. Hormone therapies have long been used to treat prostate cancer and have indeed helped improve outcomes for many patients. However, a major challenge has been the development of resistance to these hormone treatments over time, which complicates long-term management.
Currently, a promising development in the fight against hormone-resistant prostate cancer is the emergence of NXP800, a novel drug. This drug is presently undergoing clinical trials and has shown potential as an effective treatment option for those whose cancer no longer responds to conventional hormone therapies. NXP800 offers hope by targeting cancer cells in ways that existing treatments do not, potentially providing a new avenue for overcoming this resistance.
As research progresses, the medical community remains hopeful that NXP800 will be a game-changer in the treatment of hormone-resistant prostate cancer, offering renewed hope and possibly extending the lives of many men affected by this challenging condition. The successful integration of NXP800 into existing treatment protocols could mark a significant step forward in the ongoing battle against prostate cancer, addressing a critical unmet need in oncology.