Small cell lung cancer (SCLC) represents one of the most formidable challenges in oncology, characterized by its aggressive nature and a disheartening prognosis that leaves many patients with limited hope. Accounting for roughly 15% of lung cancer cases, this disease spreads rapidly and often resists standard treatments, resulting in a three-year survival rate of just 15%. A groundbreaking study published in Cell Reports Medicine on June 20, 2025, conducted by researchers from the Hospital del Mar Research Institute in collaboration with the CIBERONC cancer research network, unveils a promising new approach. By targeting a specific molecular pathway known as MET, this research enhances the effectiveness of existing chemo-immunotherapy protocols, potentially transforming outcomes for SCLC patients. The findings not only tackle the persistent issue of treatment resistance but also suggest broader implications for other hard-to-treat cancers. This discovery marks a significant step forward, sparking curiosity about how such innovations might reshape cancer care in the near future.
Confronting the Severity of Small Cell Lung Cancer
The battle against small cell lung cancer remains an uphill struggle due to its rapid progression and early metastasis, often rendering surgical options unfeasible. Most patients receive a diagnosis at an advanced stage, where the disease has already spread, severely limiting the effectiveness of interventions. Standard care typically involves a combination of chemotherapy and immunotherapy, with drugs targeting immune checkpoints like PD-L1 to stimulate the body’s natural defenses. However, the temporary nature of responses to these treatments is a major concern, as resistance frequently develops, leading to disease progression in a majority of cases. This persistent challenge underscores the urgent need for novel strategies that can break through the barriers of resistance and offer sustainable benefits to those affected by this devastating form of cancer.
Equally troubling is the stark survival statistic that haunts SCLC, with only a small fraction of patients surviving beyond three years post-diagnosis. This low rate is compounded by the disease’s ability to evade even the most aggressive therapeutic regimens, often leaving clinicians with few alternatives. The complexity of SCLC lies in its biological behavior, which not only promotes swift tumor growth but also fosters an environment that hinders immune system attacks. Addressing these multifaceted issues requires a deeper understanding of the molecular drivers behind the disease’s resilience. As research continues to uncover the intricacies of SCLC, the focus shifts toward innovative therapies that can disrupt the mechanisms of resistance and provide a lifeline to patients facing limited options in their fight against this relentless malignancy.
Unraveling the MET Pathway’s Role in Resistance
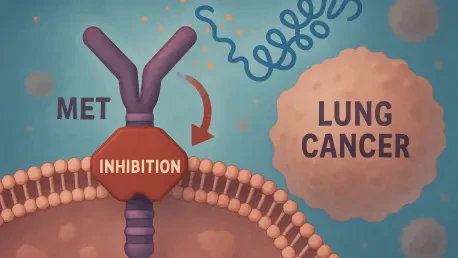
Central to the challenge of treating SCLC is the MET signaling pathway, driven by the MET gene and its ligand, hepatocyte growth factor (HGF), which significantly contributes to tumor growth and therapeutic resistance. This pathway acts as a catalyst for cancer cell proliferation, survival, and migration, while also creating an immunosuppressive shield around the tumor that dampens immune responses. Studies reveal that in approximately half of SCLC patients, MET is overactive, a condition linked to poorer clinical outcomes through analysis of human tumor samples. This discovery highlights the pathway’s critical influence on the disease’s ability to withstand conventional treatments, positioning it as a prime target for intervention.
Beyond its role in fueling cancer progression, the MET pathway’s impact on the tumor microenvironment adds another layer of complexity to SCLC management. By fostering conditions that suppress immune activity, it effectively blocks the body’s natural defenses and reduces the efficacy of therapies like immunotherapy. This dual action of promoting tumor growth while shielding it from immune attacks explains why so many patients experience relapses after initial treatment responses. Targeting this pathway offers a potential avenue to dismantle these protective barriers, thereby enhancing the overall impact of existing treatments. The focus on MET inhibition represents a shift toward addressing not just the cancer cells themselves, but the broader ecosystem that sustains their survival and resistance.
Breakthrough Strategy with MET Inhibition
A pioneering approach explored in recent research involves combining MET inhibition with standard chemo-immunotherapy to combat SCLC more effectively. In preclinical models designed to replicate human SCLC, scientists tested various treatment combinations, including chemotherapy alone, chemo-immunotherapy with anti-PD-L1 agents, and a triple regimen incorporating a MET inhibitor. The results were remarkable, with the addition of the MET inhibitor leading to significantly reduced tumor growth and improved survival rates. Notably, two-thirds of the treated cases achieved complete remission, a stark contrast to outcomes seen with conventional therapies alone, suggesting a transformative potential for this combined approach.
This innovative strategy’s success lies in its ability to address the root causes of resistance that plague SCLC treatment. Unlike single-agent therapies that often falter against the disease’s adaptive mechanisms, the integration of MET inhibition appears to create a synergistic effect, amplifying the antitumor activity of chemotherapy and immunotherapy. Such findings point to a future where multifaceted treatment plans could become the norm for managing aggressive cancers. While these results are based on preclinical data, they provide a compelling foundation for further exploration, igniting hope that this method could soon translate into tangible benefits for patients grappling with limited therapeutic avenues. The promise of complete remission in a majority of cases underscores the urgency of advancing this research to clinical settings.
Mechanism Behind MET Inhibition’s Success
The effectiveness of MET inhibition in enhancing immunotherapy stems from its unique mechanism of action, which diverges from traditional cytotoxic drugs that directly target cancer cells. Instead, MET inhibitors focus on remodeling the tumor microenvironment, breaking down the immunosuppressive barriers that protect cancer cells from immune attacks. By doing so, they enable effector T cells, activated through anti-PD-L1 immunotherapy, to penetrate the tumor more efficiently and mount a robust assault. This indirect approach amplifies the immune system’s ability to recognize and eliminate cancer cells, offering a novel way to overcome the resistance that often undermines treatment success.
Further insight into this mechanism reveals how MET inhibition addresses a critical gap in current SCLC therapies. The tumor microenvironment, shaped by the MET pathway, typically stifles immune activity, rendering checkpoint inhibitors less effective over time. Altering this environment through targeted inhibition allows for a sustained immune response, which is essential for achieving durable outcomes. This synergy between MET inhibitors and immune checkpoint blockade highlights a sophisticated interplay of molecular and immunological factors, demonstrating that effective cancer treatment requires tackling multiple dimensions of the disease. Such an understanding pushes the boundaries of therapeutic design, emphasizing the importance of integrated approaches in modern oncology.
Clinical Horizons and Next Steps
The clinical relevance of MET inhibition is reinforced by evidence from human tumor samples, which show a clear association between MET overexpression and worse prognosis in SCLC patients. This correlation, observed in about 50% of cases, suggests that a significant portion of individuals could benefit from therapies targeting this pathway. Although the research remains in the preclinical phase, it sets the stage for an anticipated clinical trial aimed at evaluating MET inhibitors during the maintenance phase of immunotherapy. The goal is to prevent tumor regrowth and extend survival, addressing a critical unmet need in the management of this aggressive cancer.
Looking ahead, the planned trial represents a pivotal moment in translating laboratory findings into real-world applications. Success in this phase could validate the preclinical outcomes and pave the way for broader adoption of MET inhibitors in SCLC treatment protocols. Additionally, the focus on the maintenance phase reflects a strategic effort to sustain therapeutic gains, a crucial aspect given the disease’s tendency to recur. As researchers and clinicians collaborate to refine this approach, the potential to improve patient outcomes becomes increasingly tangible. This step forward also serves as a reminder of the importance of rigorous testing to ensure safety and efficacy, bridging the gap between innovative concepts and practical solutions for those in need.
Expanding the Scope of Cancer Therapy
The implications of MET inhibition extend far beyond SCLC, with the MET-HGF axis implicated in various aggressive and treatment-resistant cancers. Success in preclinical models suggests that this strategy could be adapted to address other malignancies, potentially benefiting a wider patient population. This versatility underscores the importance of targeting molecular pathways that play a role across different cancer types, offering a blueprint for developing therapies with broad applicability. The approach aligns with a growing trend in oncology toward combining targeted molecular therapies with immunotherapy to achieve results that surpass the limitations of single-agent treatments.
Moreover, the emphasis on altering the tumor microenvironment reflects a paradigm shift in cancer treatment, recognizing that effective therapies must address the complex ecosystem surrounding cancer cells. This holistic perspective is gaining traction as a means to enhance treatment efficacy and overcome resistance mechanisms common to many cancers. As research progresses, the integration of MET inhibition into therapeutic frameworks could inspire similar innovations, fostering a new era of personalized medicine. The broader impact of such strategies lies in their potential to redefine how aggressive cancers are managed, providing hope for improved survival and quality of life across diverse patient groups.
Reflecting on a Path Forward
Looking back, the journey of this research from the Hospital del Mar Research Institute illuminated a critical path through the daunting landscape of small cell lung cancer treatment. The identification of the MET signaling pathway as a linchpin of resistance, coupled with the demonstrated power of its inhibition in preclinical settings, marked a turning point in addressing one of oncology’s toughest adversaries. The synergy achieved by combining MET inhibitors with chemo-immunotherapy offered a glimpse into a future where durable responses were within reach. As the medical community turned its attention to upcoming clinical trials, there was a collective anticipation for results that could confirm these findings. Moving forward, the focus should center on accelerating the translation of such innovations into clinical practice, ensuring that patients benefit from these advances. Equally important is the exploration of MET inhibition’s potential in other cancers, which could expand the horizons of cancer care and solidify the role of integrated therapies in overcoming long-standing challenges.