With a deep background in biopharmaceutical research and development, Ivan Kairatov has a keen eye for innovations that could reshape how we treat the most challenging cancers. Today, he joins us to discuss a promising new preclinical study on pancreatic ductal adenocarcinoma (PDAC), a notoriously resilient disease. We’ll explore a novel dual-targeting strategy that simultaneously attacks the cancer cell’s structural integrity and its energy production, delving into the specific mechanisms of a new compound, its performance against similar drugs, and the long road from the lab to the clinic.
Pancreatic cancer is notoriously resistant to treatment. Your research explores a dual-targeting strategy aimed at both microtubules and mitochondria. Could you explain the strategic advantage of this approach and how it might overcome the cancer’s well-known adaptability to therapy?
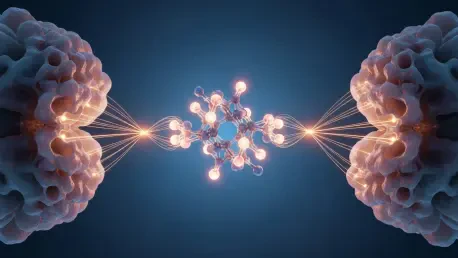
The core challenge with pancreatic cancer is its incredible resilience. It’s a master of survival, often developing resistance to therapies that target a single pathway. That’s where the dual-targeting strategy becomes so powerful. Instead of just trying to knock down one pillar, we’re targeting two fundamental systems at the same time: the cell’s physical scaffolding, its microtubules, and its power plants, the mitochondria. By attacking both the structure required for cell division and the energy supply needed to fuel all cellular processes, including resistance mechanisms, we create a crisis the cancer cell can’t easily escape. It’s a comprehensive assault that significantly reduces the cancer’s ability to adapt and survive, which is a critical step forward for a disease as aggressive as PDAC.
The compound SB-216 was shown to suppress βIII- and βIVb-tubulin expression. Can you walk us through the step-by-step impact this has on a cancer cell’s structure and ability to divide? Please share some specifics on what you observed during the cell-based assays.
Absolutely. Think of microtubules as the internal skeleton and highway system of a cell. They are made from building blocks called tubulin. During cell division, these microtubules form a critical structure called the mitotic spindle, which pulls the chromosomes apart into two new daughter cells. In our cell-based assays, we saw SB-216 directly interfere with this process. Specifically, it suppressed the expression of βIII- and βIVb-tubulin, two forms that are often overexpressed in pancreatic cancer and are linked to making the cancer resistant to other drugs. When these specific tubulins are suppressed, the microtubule network becomes unstable. The result is a direct hit to the cancer’s ability to multiply; we observed a significant reduction in cell proliferation and a clear drop in overall cell viability. The cancer cells essentially lose the structural integrity they need to divide and spread.
Beyond the structural impact, this strategy also disrupts the cancer cell’s energy supply by reducing mitochondrial oxygen consumption. What does this energy crisis signal to the cell, and what are the downstream effects of triggering processes like autophagy and mitophagy in this context?
This is the second part of the one-two punch. When we saw that SB-216 was lowering the expression of a protein called BRD4, we knew it would have consequences for the cell’s energy regulation. The resulting decrease in oxygen consumption is a clear sign that the mitochondria are failing. For a cancer cell, which is incredibly energy-hungry, this is a catastrophic signal. It triggers a state of panic, initiating self-preservation processes like autophagy—a general “self-eating” to recycle components for energy—and more specifically, mitophagy, which is the targeted removal of damaged mitochondria. While these are survival mechanisms, in this context, they are also a sign of profound cellular stress. The cell is so damaged that it’s trying to cannibalize itself to stay alive, indicating that our compound has pushed it past a critical tipping point toward cell death.
You compared SB-216 with a similar compound, Veru-111. What key differences in their mechanisms or effects led to SB-216 demonstrating a stronger and more sustained reduction in pancreatic cancer cell viability? Please provide some details on its superior performance.
Both compounds act on similar targets, which makes the comparison very informative. While Veru-111 also showed activity, SB-216 was demonstrably more potent in our model. In the lab, when we treated PDAC cells, we observed that the reduction in cell viability caused by SB-216 was not only stronger but also more durable over time. This suggests that SB-216’s dual action on both microtubules and mitochondria is perhaps more synergistic or potent. It doesn’t just wound the cell; it delivers a more decisive blow that the cell struggles to recover from. This sustained effect is exactly what you want to see in preclinical research, as it hints at a potential for more lasting therapeutic impact and a lower chance for the cancer to rebound.
These promising results were generated in a lab setting. What are the most significant hurdles and key milestones you anticipate when translating this in vitro research into animal models? What specific safety and efficacy markers will you be looking for in vivo?
The leap from a petri dish to a living organism is the most critical and challenging step in drug development. The first major hurdle is toxicity. A compound can be brilliant at killing cancer cells, but if it also harms healthy tissue, it’s a non-starter. So, our primary focus in vivo will be on establishing a safe therapeutic window. We’ll be looking for markers of liver, kidney, and bone marrow health. On the efficacy side, the key milestone will be demonstrating tumor regression in animal models of pancreatic cancer. We’ll measure tumor size, look for a reduction in metastatic spread, and analyze biomarkers from the tumor tissue to confirm that the drug is hitting its targets—suppressing tubulin expression and disrupting mitochondrial function—just as it did in vitro. Seeing these effects in a complex biological system is the green light for further development.
What is your forecast for the development of multi-targeted therapies for pancreatic cancer over the next decade?
I am incredibly optimistic. I believe the future of pancreatic cancer treatment lies precisely in this multi-targeted approach. The era of single-pathway inhibitors is giving way to more sophisticated strategies that recognize the complexity and adaptability of cancer. Over the next decade, I forecast we will see a surge in the development of dual- and even triple-action compounds like SB-216. We will also see more intelligent combination therapies, where existing drugs are paired to create synergistic attacks on different cancer hallmarks. The integration of advanced genomics and proteomics will allow us to identify the most vulnerable sets of targets for each patient’s specific tumor, moving us closer to truly personalized and overwhelmingly effective therapies for this devastating disease.