The battle against cancer is often depicted as a prolonged war of attrition, where treatments gradually weaken a tumor over time until it finally succumbs. But new research is uncovering a startling truth about ovarian cancer: the enemy’s most sophisticated defense shield may deploy the moment the first shot is fired. A groundbreaking study reveals that some cancer cells possess an innate, rapid-response survival kit, allowing them to withstand powerful drugs from the outset. This discovery challenges long-held assumptions about drug resistance and, more importantly, illuminates a new path toward dismantling this defense before it can ever fully engage, offering renewed hope in the fight against a notoriously resilient disease.
This finding is particularly critical for ovarian cancer, a malignancy that often remains hidden until its advanced stages. For years, a class of drugs known as PARP inhibitors has been a beacon of progress, especially for patients with specific genetic vulnerabilities like BRCA mutations. Yet, the initial success of these therapies is frequently overshadowed by the inevitable emergence of resistance, turning a promising treatment into a race against time. The research offers a crucial insight: by understanding how cancer cells survive the initial therapeutic onslaught, it may be possible to develop strategies that not only treat the cancer but also proactively prevent its escape, transforming the standard of care.
A Cancer’s Deadliest Defense Mechanism May Activate on Day One
The conventional understanding of drug resistance in cancer therapy has long been rooted in the principles of Darwinian evolution. According to this model, resistance is a slow, gradual process. A handful of cancer cells, by random chance, possess genetic mutations that allow them to survive treatment. As the therapy eliminates the more vulnerable cells, these few resistant ones multiply, eventually leading to a tumor that no longer responds to the drug. This process was thought to unfold over months or even years of sustained treatment.
However, recent findings from Mayo Clinic researchers turn this established theory on its head. Their work suggests that for ovarian cancer, resistance is not always a slow, adaptive creep. Instead, cancer cells can activate a pre-programmed, rapid-fire survival mechanism almost instantly upon exposure to a PARP inhibitor. This is not a matter of gradual selection but an immediate, adaptive response that enables a larger population of cancer cells to tolerate the therapeutic assault from the very beginning. This “adaptive survival response” acts as an emergency shield, giving the cells the time they need to develop more permanent forms of resistance later on.
The PARP Inhibitor Paradox a Lifeline That Fights a Losing Battle
PARP inhibitors represent one of the most significant advancements in ovarian cancer treatment in the last decade. These targeted therapies exploit a key weakness in certain cancer cells, particularly those with mutations in the BRCA1 or BRCA2 genes. These cells already have a faulty DNA repair system, and PARP inhibitors block one of their remaining backup pathways. This dual assault creates a catastrophic level of DNA damage that the cancer cells cannot survive, a concept known as synthetic lethality. For many patients, these drugs have extended remission and improved quality of life.
Despite this initial promise, the clinical reality is often a story of diminishing returns. The paradox of PARP inhibitors is that their remarkable effectiveness is frequently short-lived. A significant number of tumors eventually find ways to circumvent the drug’s mechanism, developing resistance and resuming their relentless growth. This acquired resistance stands as the single greatest obstacle to long-term survival for many ovarian cancer patients. The battle against the disease becomes a frustrating cycle of response followed by relapse, highlighting the urgent need for strategies that can either prevent or overcome this therapeutic roadblock.
Rewriting the Rules of Engagement Key Findings from the New Study
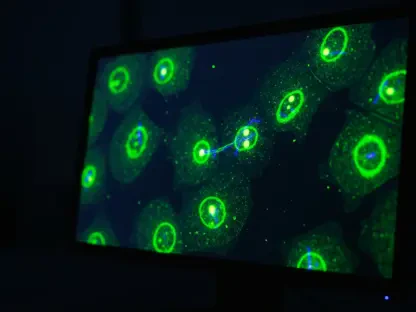
The Mayo Clinic study systematically dismantled the old rules of engagement by identifying the molecular machinery behind this rapid defense. Researchers discovered that upon exposure to a PARP inhibitor, ovarian cancer cells immediately ramp up the activity of a specific protein, a transcription factor named FRA1. Acting like a five-star general in a crisis, FRA1 sounds the alarm and activates a cascade of pro-survival genes. This orchestrated response effectively rewires the cell’s internal circuitry, allowing it to weather the storm induced by the drug and sidestep programmed cell death.
Armed with this knowledge, the research team developed a novel counter-strategy: what if they could disarm this general before the alarm is even sounded? They turned to brigatinib, a medication currently approved for treating certain types of lung cancer. Their hypothesis was that by combining a PARP inhibitor with brigatinib, they could launch a two-pronged attack, one targeting the cancer’s DNA repair weakness and the other neutralizing its immediate survival response. Preclinical experiments validated this approach with remarkable success. The combination therapy was significantly more effective at killing ovarian cancer cells than either drug alone, suggesting a powerful new synergy.
Voices from the Lab Expert Insight on Targeting Resistance Early
This research represents a fundamental change in how scientists think about therapeutic resistance. “Drug resistance does not always emerge slowly over time,” explained Dr. Arun Kanakkanthara, a senior author of the study. This statement captures the essence of the paradigm shift. Instead of reacting to resistance after it has already taken hold, the focus can now shift toward anticipating and preempting it. The discovery of the FRA1-driven survival program provides a tangible target, opening the door for proactive therapeutic strategies designed to make initial treatments more durable and effective from the start.
This new understanding has immediate clinical implications, suggesting a move away from a reactive to a proactive model of care. Dr. John Weroha, a medical oncologist at Mayo Clinic and co-senior author, emphasized this point, noting the importance of “targeting resistance early, before it has a chance to take hold.” A proactive approach could fundamentally alter the treatment trajectory for patients. By using a combination therapy upfront, clinicians might prevent the cancer from ever gaining a foothold of resistance, potentially leading to deeper, more lasting remissions and improving long-term outcomes for those battling this challenging disease.
From Preclinical Promise to a Patient Focused Strategy
Further investigation into how the drug combination worked yielded another surprise. The efficacy of brigatinib was not related to traditional DNA repair pathways, but to a previously unrecognized mechanism. The study revealed that brigatinib simultaneously shuts down two critical signaling molecules that aggressive ovarian cancer cells rely on for survival: Focal Adhesion Kinase (FAK) and EPH Receptor A2 (EPHA2). By delivering this dual blockade, brigatinib dismantles a core part of the cancer cell’s survival infrastructure, leaving it profoundly vulnerable to the PARP inhibitor’s primary assault.
Crucially, this potent cell-killing effect was highly selective. The combination therapy demonstrated a remarkable ability to eliminate cancerous cells while leaving normal, healthy cells largely unharmed. This selectivity is a critical attribute for any successful cancer therapy, as it promises greater efficacy with fewer debilitating side effects for patients. It suggests that this combination could be both more powerful and more tolerable than existing regimens.
This research did more than just propose a new treatment; it also laid the groundwork for a personalized, patient-focused strategy. The team observed that tumors with naturally high levels of FAK and EPHA2 were the most sensitive to the combination therapy. This finding suggests that these two molecules could serve as powerful predictive biomarkers. By measuring their levels in a patient’s tumor, oncologists could one day identify individuals most likely to benefit from this targeted approach, ensuring that this promising therapy is delivered to the patients who need it most. The insights from these preclinical studies have provided a robust foundation for a new therapeutic strategy that could significantly improve the lives of those affected by ovarian cancer.