In the persistent and complex war against cancer, one of the greatest hurdles has always been the enemy’s cunning ability to evade destruction, but a newly unveiled biological process, termed triaptosis, offers a groundbreaking strategy to circumvent this resistance by inducing a novel form of cellular self-destruction. This discovery, first detailed in a pivotal study and further explored in subsequent reviews, is generating significant excitement within the oncology community as it addresses a fundamental challenge in cancer therapy: the failure of conventional treatments due to the remarkable resilience of malignant cells. For countless patients, treatment resistance remains a devastating reality, where tumors that initially respond to therapy eventually evolve to ignore the cell-killing signals of chemotherapy and radiation. By targeting a previously unknown vulnerability, triaptosis presents a fresh therapeutic avenue that could potentially redefine treatment paradigms for some of the most stubborn cancers, providing a powerful new weapon in a long-fought battle against an evolving disease.
Unraveling the Triaptosis Mechanism
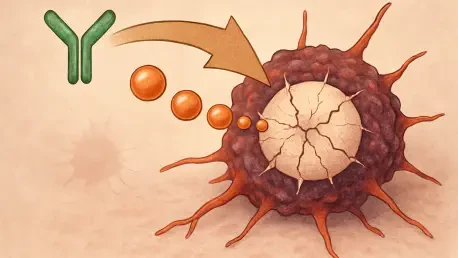
The mechanism of triaptosis is fundamentally distinct from all previously characterized forms of programmed cell death, such as apoptosis or necroptosis, setting it apart as a unique and potentially more effective process. The pathway is initiated by menadione, a synthetic precursor of vitamin K, which acts not as a nutrient but as a potent pro-oxidant within the cellular environment. This compound selectively triggers the oxidation of a specific kinase known as PIK3C3, also referred to as VPS34. This particular kinase is a master regulator of the endosomal system, a complex network of internal membranes responsible for sorting and transporting cellular cargo. The oxidative damage to PIK3C3 effectively paralyzes this critical trafficking system, which cancer cells rely on heavily for their survival and rapid growth. This disruption leads to a dramatic and catastrophic cellular event: the progressive accumulation of massive, fluid-filled vacuoles inside the cell, which swell and distort its internal architecture until the pressure becomes unbearable, culminating in the complete rupture of the outer plasma membrane and the ultimate demise of the cell.
The therapeutic promise of this novel pathway was not confined to laboratory cell cultures, as compelling preclinical evidence has already demonstrated its potent anti-tumor activity in living organisms. In a significant mouse model study involving aggressive prostate cancer, researchers administered menadione orally to induce triaptosis within the tumors. The results were striking, showing that this approach achieved superior tumor control when compared directly against standard-of-care treatments for this type of cancer. Furthermore, the treatment exhibited a highly favorable safety profile, with minimal adverse effects observed in the animal models. This combination of high efficacy and low toxicity is a critical milestone in drug development, underscoring the significant translational potential of triaptosis. These findings provide a strong rationale for advancing this strategy toward human clinical trials, suggesting that what works in a preclinical setting could one day offer a viable and safer alternative for patients who have exhausted other treatment options, moving this innovative approach one step closer to the clinic.
Harnessing a New Therapeutic Strategy
The profound efficacy of triaptosis stems from its ability to exploit a fundamental vulnerability inherent to many types of cancer, often described as the disease’s “Achilles’ heel.” Malignant cells are defined by their rapid and uncontrolled proliferation, a process that places an enormous demand on their internal machinery. To sustain this growth, they become heavily dependent on their endomembrane trafficking system for nutrient uptake, waste removal, and signaling. By specifically disabling the PIK3C3/VPS34 kinase, triaptosis strikes at the very heart of this hyperactive system, effectively cutting off the supply lines that cancer cells need to survive and multiply. Moreover, because this pathway operates independently of the canonical apoptotic machinery that many existing chemotherapies rely on, it holds immense potential for overcoming treatment resistance. This makes triaptosis a particularly valuable strategy for patients whose tumors have evolved to evade conventional cell death signals, positioning it as a vital last-line therapeutic option when other treatments have failed to halt disease progression.
Beyond its direct cell-killing capabilities, the discovery of triaptosis opens up exciting possibilities for synergy with one of the most powerful modern cancer treatments: immunotherapy. The endosomal system, which is the direct target of triaptosis, plays a central role in a critical immune process known as antigen presentation. This is how cells display fragments of internal proteins on their surface for surveillance by the immune system. By inducing the chaotic collapse of the endosomal network, triaptosis could potentially trigger a more robust presentation of tumor-specific antigens, effectively unmasking the cancer to immune cells. This could help convert immunologically “cold” tumors, which are invisible to the immune system, into “hot” tumors that can be readily attacked. Such a transformation would significantly enhance the efficacy of immune checkpoint inhibitors, a class of drugs that works by releasing the brakes on the immune system, allowing it to mount a powerful and specific antitumor response where it previously could not, thereby broadening the potential impact of this novel cell death pathway.
Paving the Path to Clinical Application
The groundbreaking identification of triaptosis marked a pivotal moment, shifting the scientific focus from a biological curiosity to a tangible clinical objective. The path forward was immediately defined by several key research imperatives aimed at translating this discovery from the laboratory to the clinic. Primary among these objectives became the identification and development of novel chemical agents capable of inducing triaptosis with greater efficiency and selectivity than menadione. To maximize the therapeutic window, research efforts also pivoted toward engineering intelligent drug delivery systems, such as nanoparticles, designed for precise tumor targeting to minimize systemic side effects. Scientists recognized the importance of elucidating the intricate crosstalk between triaptosis and other cell death modalities, like ferroptosis, which opened avenues for designing sophisticated combination therapies to preemptively overcome resistance. This discovery not only broadened the fundamental understanding of cellular life and death but also offered renewed hope by laying the groundwork for innovative treatments that could soon bridge the clinical gap for cancer patients.