In the battle against infectious diseases like tuberculosis (TB) and malaria, which claim nearly 2 million lives each year in low- and middle-income countries (LMICs), clinical trials serve as a critical frontline for developing life-saving treatments and preventive measures. These regions, often burdened with the highest disease prevalence, face unique challenges that make trial execution far from straightforward. From limited healthcare infrastructure to cultural and ethical complexities, ensuring safety and efficacy in these settings demands a nuanced approach. The stakes are high, as ineffective or unsafe interventions can exacerbate already dire health crises. This article delves into the intricate landscape of conducting clinical trials in LMICs, spotlighting the efforts of organizations like the Gates Medical Research Institute to address safety concerns while tailoring solutions to local realities. By examining key aspects such as pharmacokinetics, inclusivity of vulnerable populations, and capacity building, a clearer picture emerges of how to balance scientific rigor with the urgent needs of communities most affected by these global health threats.
Deciphering Drug Dynamics in Diverse Settings
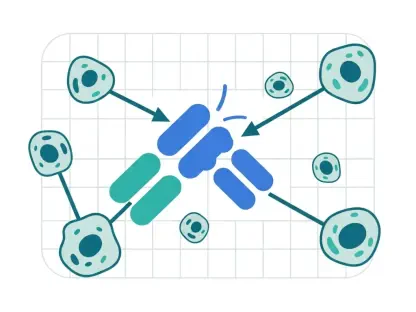
Understanding how drugs interact with the human body is a foundational element in developing treatments for TB and malaria, particularly in LMIC populations where variability is the norm. Pharmacokinetics (PK), which analyzes how the body absorbs, distributes, metabolizes, and excretes a drug, alongside pharmacodynamic (PK/PD) relationships that connect drug exposure to therapeutic or adverse effects, forms the bedrock of safe dosing strategies. In LMICs, factors such as genetic differences, dietary habits, and coexisting health conditions can dramatically influence these processes. For instance, malnutrition, a common issue in many high-burden areas, may alter drug absorption rates, necessitating specialized studies to ensure treatments remain effective. Without accounting for such diversity, there’s a risk that therapies developed in controlled environments may fail when applied in real-world LMIC contexts, potentially leading to ineffective care or harmful side effects.
The use of mathematical models derived from PK/PD data offers a powerful tool to predict outcomes in untested scenarios, streamlining trial designs and optimizing dose selection for varied populations. Conducting trials across multiple regions within LMICs ensures a comprehensive grasp of a drug’s behavior, which is indispensable for securing regulatory approval and achieving meaningful impact. This approach not only enhances the safety profile of new interventions but also builds confidence that treatments will perform as intended in the communities that need them most. By prioritizing such detailed research, the global health community can avoid the pitfalls of one-size-fits-all solutions, paving the way for therapies that are both scientifically sound and practically applicable in resource-limited settings.
Overcoming Barriers in Resource-Limited Environments
Clinical trials in LMICs must navigate a complex web of challenges stemming from both global and local regulatory expectations, often requiring protocols that meet stringent international standards while remaining flexible to regional constraints. Limited healthcare infrastructure, economic hardships, and logistical difficulties frequently complicate trial implementation, from patient recruitment to data collection. Excluding these communities from research would be a grave misstep, as it would hinder progress in reducing disease incidence and mortality where the burden is heaviest. Instead, trials must be designed with inclusivity at their core, ensuring that data generated reflects the realities of those most affected by TB and malaria, even when resources are scarce or access to care is inconsistent.
Cultural sensitivities add another layer of complexity to trial execution in LMICs, as differing beliefs and practices can influence participant engagement and adherence to protocols. Building trust within communities becomes paramount, often requiring extensive outreach and education to align trial objectives with local values. For example, addressing misconceptions about medical research or ensuring informed consent processes respect cultural norms can significantly impact trial success. Tackling these barriers involves not just logistical planning but a deep commitment to understanding the social fabric of each region, ensuring that interventions are not only scientifically valid but also accepted and sustainable within the communities they aim to serve.
Prioritizing Safety for At-Risk Populations
When it comes to including vulnerable groups such as women of childbearing potential and pregnant women in clinical trials for TB and malaria, safety considerations take on heightened importance in LMIC settings. These populations often face greater risks from these diseases, yet they are frequently excluded from early-phase research due to potential harm to themselves or their fetuses. A cautious, phased approach is advocated, where inclusion in later trial stages occurs only after sufficient safety data from toxicology studies is available. This strategy seeks to balance the urgent need for relevant data with the ethical imperative to protect participants, ensuring that treatments are safe for those who may need them most in high-burden areas.
Beyond initial exclusion, ensuring safety during trials involves providing access to culturally appropriate contraception to prevent unintended pregnancies, while respecting local norms and religious beliefs that vary widely across regions. Historical gaps in research have left pregnant women underserved, often lacking evidence-based care for diseases like TB and malaria despite their heightened vulnerability. Addressing this requires targeted pharmacokinetic and safety studies in later phases, aimed at closing these evidence gaps. By prioritizing such efforts, the medical community can develop interventions that are not only effective but also equitable, ensuring that all demographics within LMICs receive the protection and care they deserve.
Tailoring Approaches to Local Contexts
Clinical trials in LMICs must account for a range of local realities that can profoundly affect outcomes, from nutritional challenges to social stigma surrounding diseases like TB. For instance, some drugs require food for optimal absorption, raising ethical dilemmas in food-insecure regions where providing meals might be perceived as an inducement to participate. Similarly, undernutrition, a known risk factor for TB, complicates trial design and interpretation of results. Stigma also poses a barrier, as traditional directly observed therapy for TB can inadvertently disclose a patient’s diagnosis, leading to social ostracism. Innovative solutions, such as video-based monitoring via mobile devices, offer a way to maintain adherence while preserving patient dignity, provided such tools are not seen as incentives.
Healthcare capacity in many LMIC trial sites often falls short of what’s needed to manage adverse events or complex patient needs, making site selection a critical decision. Investments in improving facilities or training local staff can bridge these gaps, ensuring safer trial environments. Additionally, each trial presents an opportunity to build lasting research capacity, addressing the stark disparity where only a small percentage of global trials occur in regions like sub-Saharan Africa or South Asia. Aiming to increase this representation over the coming years, from the current low base to a target of 10-15% within five years, reflects a commitment to creating sustainable public health ecosystems. This dual focus on immediate trial safety and long-term infrastructure growth ensures that interventions remain relevant and impactful for the communities they target.
Fostering Sustainable Health Solutions
Reflecting on the efforts to enhance clinical trials in LMICs for TB and malaria, it’s evident that a delicate balance between scientific precision and cultural empathy shaped past endeavors. Safety protocols adapted to local variabilities, such as nutritional status and genetic differences, proved essential in safeguarding participants while yielding reliable data. The cautious inclusion of vulnerable groups, supported by culturally sensitive measures, addressed critical gaps in research, ensuring broader applicability of findings. Investments in local research capacity, though gradual, laid the groundwork for more equitable health interventions in regions long underrepresented in global studies.
Looking ahead, the path forward involves scaling these efforts through strategic partnerships and continued funding to bolster LMIC health systems. Prioritizing innovative tools, like digital monitoring for treatment adherence, can further enhance trial efficiency without compromising ethical standards. Additionally, fostering international collaboration to share best practices will help standardize safety measures across diverse settings. By committing to these actionable steps, the global health community can ensure that future trials not only mitigate the burden of TB and malaria but also empower LMIC regions with the tools and expertise needed for enduring progress.