A significant portion of cancer patients do not respond to immunotherapy because their tumors are immunologically inactive, but a groundbreaking collaborative study from Cornell University researchers has unveiled a remarkable solution using ultrasmall fluorescent silica nanoparticles, known as Cornell prime dots or C’dots. Published in the journal Nature Nanotechnology, the research demonstrates that these nanoparticles possess an astonishing and previously unknown intrinsic ability to reprogram the tumor microenvironment (TME), effectively converting treatment-resistant cancers into ones that are highly receptive to immunotherapy. This pivotal discovery reframes the role of these particles, elevating them from passive diagnostic aids and drug carriers to potent, active therapeutic agents that could revolutionize cancer treatment paradigms.
An Unforeseen Therapeutic Power
The research, a joint effort spearheaded by Dr. Michelle Bradbury at Weill Cornell Medicine and Professor Ulrich Wiesner at Cornell Engineering, yielded a finding that was described as “very surprising.” The core discovery is that C’dots, on their own and without being loaded with any pharmaceutical drug, exert a wide spectrum of anti-cancer effects. This intrinsic activity was entirely unexpected, as the nanoparticles had previously been evaluated in human clinical trials primarily for their utility in cancer diagnostics and as a sophisticated drug delivery system. This revelation was critically informed by the expertise of Dr. Jedd Wolchok and Dr. Taha Merghoub, who provided deep insights into animal models and the complex dynamics of the TME. The finding fundamentally alters the scientific community’s perception of these materials, suggesting that the vehicle itself can be as therapeutically important as the cargo it was designed to carry, opening a new frontier in nanomedicine.
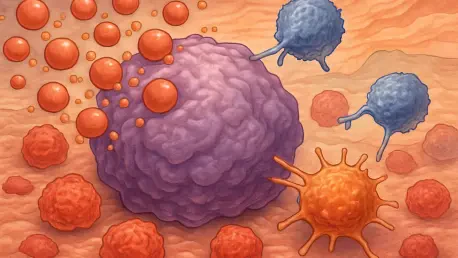
The latest findings significantly expand upon a 2016 study where the team first noted that C’dots could trigger a specific form of regulated cell death known as ferroptosis, thereby inhibiting tumor growth without conventional chemotherapy. The new research unveils a far more intricate and powerful mechanism of action. Using aggressive melanoma models notorious for their resistance to immunotherapy, the scientists discovered that C’dots orchestrate a simultaneous, multi-pronged attack on the cancer. The nanoparticles were observed stimulating the body’s innate immune defenses via pattern-recognition receptors, inducing cell-cycle arrest to halt the proliferation of malignant cells, alleviating the profound immune suppression characteristic of the TME, and fundamentally reprogramming key immune cells, such as T cells and macrophages, to more effectively recognize and eradicate cancer cells. This multifaceted approach represents a holistic assault on tumor biology that is difficult to achieve with traditional, single-target drugs.
Overcoming Immunotherapy Resistance
A central challenge in modern oncology is the nature of aggressive solid tumors, including many melanomas, as well as prostate, breast, and colon cancers, which often create an immunologically “cold” microenvironment. This “cold” state signifies a lack of the necessary immune cell infiltration and inflammatory signals required for the body to mount a strong anti-tumor response, rendering powerful treatments like immunotherapy largely ineffective. The study compellingly shows that the administration of C’dots can effectively transform these non-responsive “cold” tumors into “hot” ones. By doing so, they generate an inflamed, immune-receptive environment where immunotherapies can finally function with dramatically improved efficacy. As Dr. Bradbury emphasized, this platform is not merely a passive carrier; these nanoparticles are “intrinsically active therapeutic agents” that engage multiple biological mechanisms at once in a manner that is exceedingly difficult to replicate with standard pharmaceutical interventions.
To validate these groundbreaking observations, the research team developed and tested a novel combinatorial treatment strategy within sophisticated mouse models. They administered the C’dots in conjunction with a dual immunotherapy regimen that simultaneously targeted both a critical immune checkpoint and a cytokine, a type of signaling molecule that helps regulate immune responses. The results of this combination therapy were profound, producing a significant survival advantage when compared to the outcomes of using immunotherapy alone. The researchers characterized the outcome as a “synergistic one-two punch.” In this sequence, the nanoparticles first modulate the immune landscape to effectively prime the tumor, after which the subsequent immunotherapy is able to deliver a much more powerful and therapeutically effective blow. This strategy successfully mitigates the inhibitory activities within the TME, which in turn suppresses tumor growth and limits the development of treatment resistance.
A New Therapeutic Paradigm
The implications of this research extended far beyond melanoma. The Weill Cornell Medicine team observed similar immune-activating properties of C’dots in other solid tumor models, including prostate and ovarian cancers, suggesting a broad potential for this innovative approach across various cancer types. Further reflection on these results led Professor Wiesner to posit a deeper, evolutionary hypothesis for silica’s remarkable biological activity. He noted that for millions of years, organisms have been internally exposed to nanoparticulate silica through their diet, consuming it in foods such as grasses and seaweed. The hypothesis proposed that while cancer pushes the body’s systems away from a state of equilibrium, or homeostasis, silica nanoparticles may act to “push back.” According to this speculative but intriguing theory, the multifaceted anti-cancer effect of C’dots may have stemmed from various mechanisms that organisms evolved over eons to utilize silica for maintaining homeostasis. This novel idea, which connects nanomedicine to evolutionary biology, was explored further in collaboration with researchers in nutritional sciences at Cornell, funded by the National Institutes of Health and the Parker Institute for Cancer Immunotherapy.