Diving into the forefront of cancer immunotherapy, we’re thrilled to speak with Ivan Kairatov, a renowned biopharma expert with extensive experience in research and development. Ivan’s deep knowledge of technological innovation in the industry has positioned him as a leading voice in the fight against HPV-related cancers. Today, we’ll explore a groundbreaking nanoparticle vaccine that has shown remarkable promise in eradicating tumors in animal models, discuss its potential to transform treatment for metastatic cancers, and uncover what this could mean for patients in the future.
Can you start by explaining what this nanoparticle vaccine is and how it works to fight HPV-related cancers?
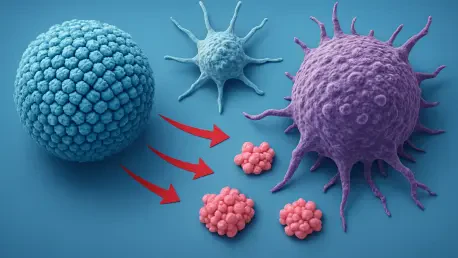
Absolutely. This nanoparticle vaccine is a cutting-edge therapeutic approach designed to target cancers caused by the human papillomavirus, or HPV. It’s not a preventive vaccine like the ones we have for HPV infection, but rather a treatment for existing cancers. The vaccine uses tiny particles, about 25 to 30 nanometers in size, to deliver specific components that activate the immune system. Once injected, these particles are taken up by immune cells, particularly in the spleen, where they unpack their cargo. This triggers a powerful immune response that seeks out and attacks cancer cells carrying HPV-specific markers, essentially training the body to fight the disease from within.
What are the key components in this vaccine that help stimulate such a strong immune response?
The vaccine combines a few critical elements. First, there’s a polymer and a small-molecule drug that work together to activate a protein called STING, which plays a big role in boosting immune activity. Then, we include a protein antigen called E7, which is derived from HPV. This E7 protein acts like a red flag for the immune system, helping it recognize and target cells infected with HPV or turned cancerous because of it. Together, these components, encapsulated in nanoparticles, create a one-two punch that both alerts and directs the immune system to the cancer.
Why is this vaccine considered a game-changer compared to current treatments for HPV-related cancers?
Current treatments for HPV-related cancers, like cervical or head and neck cancers, often rely on surgery, radiation, or chemotherapy. These can be effective for early-stage or localized tumors, but they come with significant limitations. When the cancer has spread to other organs or is in a location that’s hard to access surgically, these options often fall short. This vaccine offers a systemic approach, meaning it works throughout the body to target both primary tumors and metastatic nodules. It’s a way to address cancers that are otherwise untreatable with conventional methods, potentially offering hope to patients with advanced disease.
Can you walk us through the results you observed in animal studies with this nanovaccine?
The results in our mouse models were incredibly encouraging. We tested the vaccine in mice with HPV-related tumors, including models of metastatic lung cancer. What we saw was that the vaccine not only shrank the primary tumors but also eliminated metastatic nodules that had spread to other organs. About 71% of the treated mice were still alive 60 days after treatment, which is a stark contrast to the groups receiving standard treatments like immune checkpoint inhibitors, where survival was much lower. It was clear evidence of the vaccine’s potential to tackle late-stage disease.
What happened when you combined this nanovaccine with checkpoint therapy?
Combining the nanovaccine with checkpoint therapy was a revelation. Checkpoint inhibitors are drugs that help unleash the immune system by removing certain brakes on it, but on their own, they didn’t perform as well in our models. When we paired them with the nanovaccine, we saw a synergistic effect—100% of the mice survived the 60-day period. This suggests that the vaccine could enhance existing therapies, creating a more robust attack on the cancer by leveraging multiple immune pathways.
Safety is always a concern with new treatments. How did the nanovaccine hold up in terms of side effects in these studies?
Safety was a top priority for us, and the results were reassuring. In the animal studies, we didn’t observe any significant side effects. There was no organ damage, no noticeable weight loss, and no signs of systemic toxicity. The immune response seemed to be tightly focused on the cancer cells, without triggering unwanted inflammation or damage elsewhere in the body. This specificity is crucial for a therapeutic vaccine, and it gives us confidence as we think about moving forward to human trials.
What sets this nanovaccine apart from other therapeutic vaccines being developed for cancer?
What makes this approach unique is the combination of the STING activator and the HPV-specific E7 protein, delivered via nanoparticles. The STING pathway is a powerful way to amplify the immune response, almost like sounding an alarm to wake up the immune system. Pairing that with E7 ensures the response is targeted to HPV-driven cancers. The nanoparticles themselves are also key—they protect the components, ensure they reach the right immune cells, and release them in a controlled way. This delivery system, combined with the specific immune triggers, sets our vaccine apart from other strategies that might not have this level of precision or potency.
HPV-related cancers impact so many lives. How close are we to seeing this vaccine tested in humans?
We’re still in the preclinical stage, so there’s work to be done before we can start human trials. The next steps involve more extensive testing in animal models to confirm the efficacy and safety across different scenarios and cancer types. We also need to optimize the formulation and dosing to ensure it’s ready for clinical settings. After that, we’ll move toward regulatory approvals to begin Phase 1 trials in patients, which would focus on safety and initial efficacy. While it’s hard to predict an exact timeline, each successful study brings us closer to the goal of helping patients with these devastating cancers.
What is your forecast for the future of nanoparticle-based therapies in cancer treatment?
I’m incredibly optimistic about the future of nanoparticle-based therapies. They offer a level of precision and versatility that’s hard to achieve with traditional treatments. In the coming years, I believe we’ll see more tailored approaches, where nanoparticles are customized to deliver not just vaccines but also drugs or genetic material directly to cancer cells. For HPV-related cancers specifically, I think therapeutic vaccines like this one could become a cornerstone of treatment, especially for advanced cases. As we refine the technology and better understand the immune system, I expect these therapies to play a major role in turning cancer into a manageable, if not curable, condition.