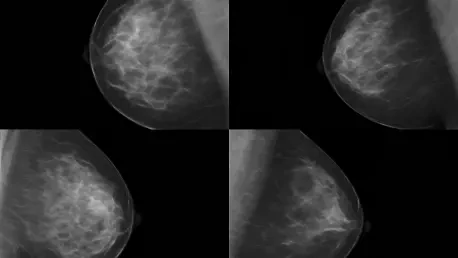
I’m thrilled to sit down with Ivan Kairatov, a renowned biopharma expert with extensive experience in research and development, particularly in innovative technologies shaping the future of healthcare. Today, we’re diving into a groundbreaking study from UCLA Health on the impact of regular mammograms for women over 80—a topic that’s long been shrouded in uncertainty. Our conversation will explore why this age group has been overlooked in screening guidelines, the surprising benefits of continued mammography, and how early detection can transform treatment and survival outcomes. We’ll also touch on the challenges of balancing benefits against risks like overdiagnosis, and what this means for older women and their healthcare providers.
Can you start by sharing what motivated researchers to focus on the benefits of mammograms for women over 80?
Absolutely, Julia. The inspiration behind studying this age group stems from a significant gap in medical guidelines and data. Most breast cancer screening recommendations stop at age 74, leaving women 75 and older in a gray area. With the population of older adults growing rapidly in the U.S., and knowing that age is a major risk factor for breast cancer, it became critical to understand whether screening could still make a difference for women in their 80s. We wanted to provide clarity for both patients and doctors who often face tough decisions without solid evidence to guide them.
Why do you think there’s been so little clear guidance on breast cancer screening for women over 75?
That’s a great question. One big reason is the historical lack of research focused on this age group. Older women are often underrepresented in clinical trials due to concerns about other health conditions or shorter life expectancy, which can complicate study design. There’s also a hesitation around potential harms like overdiagnosis or the stress of unnecessary tests. Without robust data, guidelines remain vague, leaving decisions to individual providers. This uncertainty can lead to inconsistency in care—some women might miss out on lifesaving screenings, while others might undergo procedures they don’t need.
Your study found that women in their 80s who get regular mammograms have better outcomes. Can you explain what ‘better outcomes’ really means for these patients?
Sure. ‘Better outcomes’ primarily refers to detecting breast cancer at an earlier stage, which is often less aggressive and easier to treat. In our study, women who were screened typically had stage 1 or 2 cancers, compared to more advanced tumors in those who weren’t screened. Beyond early detection, this translated to higher survival rates—a 74% lower risk of dying from breast cancer among screened women. It’s not just about living longer, though; it’s about maintaining a better quality of life through less invasive treatments, which I’m happy to dive into further.
Speaking of treatments, how does early detection through mammograms help reduce the intensity of care needed for these older women?
Early detection is a game-changer because it often means the cancer hasn’t spread or grown significantly. For many postmenopausal women with hormone-sensitive breast cancers, which are common in this age group, catching it early can mean avoiding heavy-duty treatments like chemotherapy or radiation. Sometimes, even sentinel lymph node biopsy can be skipped. Instead, a simple surgery to remove the tumor might be enough. This reduction in treatment intensity is huge for older patients—it minimizes physical strain, recovery time, and emotional stress, allowing them to maintain their daily routines more easily.
The numbers in your study are striking—a 55% lower risk of cancer returning and a 74% lower risk of dying for screened women. Why do these figures stand out to you?
Honestly, these numbers were surprising even to us. We knew screening would likely show benefits, but the magnitude of the difference was remarkable. A 74% lower risk of death highlights just how powerful early detection can be, even in an older population where other health issues might complicate outcomes. Compared to younger age groups, where survival benefits are well-documented, these stats suggest that the impact of screening doesn’t diminish with age as much as we might have assumed. It’s a strong argument for not arbitrarily stopping mammograms based on a birthday.
Since age is a major risk factor for breast cancer, can you unpack why older women are at such a high risk?
Certainly. As women age, the cumulative exposure to hormones like estrogen over decades increases the likelihood of cellular changes in breast tissue that can lead to cancer. The risk doesn’t necessarily level off—it continues to climb into the 80s and beyond, though the rate of increase might slow. Other factors play a role too, like family history, lifestyle, or even just the natural aging of the immune system, which might not catch abnormal cells as effectively. For women in their 80s, this combination makes regular screening even more critical to catch issues before they become serious.
There’s a concern about overdiagnosis in older women—finding cancers that might never cause harm. How do you balance this risk with the benefits of screening?
That’s a valid concern and one we wrestled with in our study. Overdiagnosis can lead to unnecessary stress, tests, or treatments, which is why our research focused on women already diagnosed with breast cancer to assess real outcomes. While we couldn’t fully capture false positives or emotional tolls in this retrospective analysis, the clear survival benefits suggest screening does more good than harm for most. Moving forward, we need larger studies to refine who benefits most and to develop tools that help distinguish between cancers that need treatment and those that don’t. It’s about personalizing care—screening shouldn’t be a one-size-fits-all approach.
What is your forecast for the future of breast cancer screening guidelines for older women based on these findings?
I’m optimistic that studies like ours will push for more specific, evidence-based guidelines for women over 75. I foresee a shift toward individualized recommendations, factoring in a woman’s overall health, life expectancy, and personal preferences, rather than a hard age cutoff. With the aging population growing, there’s also likely to be more investment in research to address lingering questions about overdiagnosis and cost-effectiveness. Ultimately, I hope we’ll see a future where every woman, regardless of age, has access to clear information and support to make informed decisions about screening.