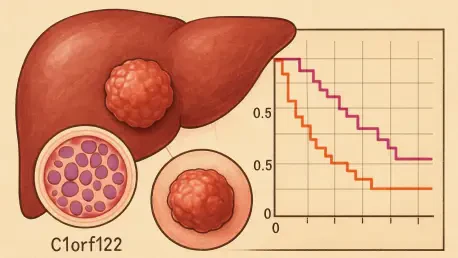
Imagine a disease so pervasive that it ranks as the third leading cause of cancer-related deaths worldwide, with a staggering 90% of primary liver cancer cases falling under its umbrella. Hepatocellular carcinoma (HCC) presents an immense challenge to global health systems, with rising incidence rates and a dire need for innovative solutions. As researchers and clinicians grapple with late-stage diagnoses and limited therapeutic options, the search for reliable biomarkers and targets intensifies. This report dives into a promising avenue of research centered on a protein-coding gene, C1orf122, which could redefine how HCC prognosis and treatment are approached in the medical field.
The current state of the HCC landscape reveals a pressing demand for advancements in early detection and personalized care. With many patients diagnosed at advanced stages, survival rates remain dishearteningly low, and existing treatments often fall short against the disease’s aggressive nature. The industry stands at a critical juncture, where molecular insights could pave the way for transformative diagnostic tools and therapies. This analysis explores how emerging genetic markers, particularly C1orf122, are shaping the future of HCC management and driving hope for better patient outcomes.
Delving into Hepatocellular Carcinoma and Biomarker Needs
Hepatocellular carcinoma dominates the realm of liver cancers, constituting the vast majority of cases and posing a significant burden on healthcare systems globally. Its status as a leading cause of cancer mortality underscores the urgency for breakthroughs in understanding its molecular underpinnings. Factors such as chronic liver diseases, viral infections, and lifestyle contributors continue to fuel its prevalence, making it a priority for oncological research and clinical innovation.
One of the most significant hurdles in managing HCC lies in the frequent occurrence of late-stage diagnosis, where therapeutic interventions have limited efficacy. Current diagnostic methods often fail to detect the disease early, and treatment options like surgery or targeted therapies are not viable for all patients. This gap highlights the critical need for molecular biomarkers that can signal the presence or progression of HCC before it reaches advanced stages, offering a window for more effective intervention.
The exploration of novel markers such as C1orf122 comes at a time when the industry is increasingly focused on precision medicine. Reliable prognostic indicators could enable clinicians to stratify patients based on risk, tailoring monitoring and treatment plans accordingly. This report examines how such biomarkers might address longstanding challenges in HCC management, setting the stage for a deeper look into a specific gene’s potential to change the game.
Exploring C1orf122 as a Pivotal Element in HCC Studies
Core Insights into C1orf122’s Impact on HCC
Recent research has spotlighted C1orf122, a protein-coding gene, as a significant factor in HCC progression, with data showing its overexpression in cancerous liver tissues compared to healthy ones. Validation through comprehensive datasets like The Cancer Genome Atlas (TCGA) and experimental studies in cell lines such as HepG2 and HuH-7 confirms this trend. Such findings suggest that C1orf122 could serve as a distinguishing feature of HCC, opening new avenues for diagnostic development.
Further analysis reveals a troubling link between elevated C1orf122 levels and diminished survival rates among HCC patients. This correlation positions the gene as a potential independent marker for prognosis, capable of identifying individuals at higher risk of poor outcomes. For the industry, this insight could translate into tools that guide clinical decision-making, prioritizing aggressive treatments for those with heightened expression levels.
Functionally, C1orf122 appears to drive tumor growth by enhancing cell proliferation, suppressing programmed cell death, and boosting migration through a process known as epithelial-to-mesenchymal transition (EMT). These effects collectively contribute to the aggressive behavior of HCC, making the gene a focal point for understanding disease mechanisms. The implications for therapeutic strategies are profound, as targeting these functions could slow or halt cancer advancement.
Underlying Molecular Pathways of C1orf122
At the molecular level, C1orf122 interacts with serine-arginine protein kinase 1 (SRPK1), facilitating a cascade of events that activate the PI3K/AKT/GSK3β signaling pathway via mTOR-mediated phosphorylation. This pathway is a well-known driver of cell growth and survival, often hijacked by cancer cells to sustain their unchecked expansion. Understanding this interaction provides a clearer picture of how C1orf122 fuels HCC progression.
The downstream effects of this signaling activation include an imbalance in proteins that regulate cell death, with a decrease in pro-apoptotic factors and an increase in anti-apoptotic ones. Simultaneously, the upregulation of EMT markers like N-Cadherin and Vimentin equips cancer cells with the ability to invade surrounding tissues and metastasize. These cellular changes underscore the gene’s role in promoting a malignant phenotype, presenting multiple points for potential therapeutic intervention.
For the industry, these mechanistic insights are invaluable, as they highlight specific pathways that could be disrupted to curb HCC growth. Drug development efforts might focus on inhibiting key components of this signaling cascade, offering hope for more targeted and effective treatments. As research progresses, the molecular understanding of C1orf122 continues to shape strategic directions in oncology.
Navigating Challenges in Establishing C1orf122 as a Prognostic Tool
Despite the promising data, validating C1orf122 as a dependable prognostic marker faces several obstacles. Current studies primarily rely on specific HCC cell lines and TCGA datasets, which may not capture the full spectrum of clinical diversity in HCC cases. This limitation raises questions about the generalizability of findings across varied patient populations and disease presentations.
To bridge this gap, further validation through animal models and patient-derived samples is essential. Such studies would provide a more robust understanding of C1orf122’s role in different contexts and stages of HCC, ensuring that conclusions drawn are applicable in real-world settings. The industry must prioritize these efforts to build confidence in the gene’s utility as a clinical marker.
Translation of these findings into practical applications also presents hurdles, including potential off-target effects or toxicity concerns when targeting C1orf122 therapeutically. Developing safe and effective interventions requires careful consideration of these risks, alongside rigorous testing to ensure patient safety. These challenges underscore the need for a cautious yet determined approach to integrating C1orf122 into clinical frameworks.
Clinical and Regulatory Implications of C1orf122 Research
The potential of C1orf122 as a prognostic tool could revolutionize how high-risk HCC patients are identified and managed. By pinpointing individuals with elevated expression levels, clinicians might implement closer monitoring or more intensive treatment regimens, personalizing care to improve outcomes. This capability aligns with the industry’s shift toward precision oncology, where tailored strategies are becoming the norm.
From a regulatory standpoint, integrating C1orf122-based diagnostics or therapies into clinical practice demands standardized protocols and adherence to stringent medical guidelines. Regulatory bodies will need to establish clear criteria for testing and validation to ensure reliability and consistency across healthcare settings. Collaboration between researchers, industry stakeholders, and regulators is crucial to streamline this process.
Ethical and safety considerations also play a pivotal role in advancing C1orf122-focused solutions. Developing therapies that modulate this gene or its pathways must prioritize patient well-being, minimizing adverse effects while maximizing therapeutic benefits. The industry must uphold high standards to foster trust and facilitate the adoption of these innovations in medical practice.
Charting the Path Forward for C1orf122 in HCC Treatment
Looking ahead, C1orf122 holds significant promise as a target for novel therapeutic approaches, particularly through drugs designed to interrupt the PI3K/AKT/GSK3β pathway or its downstream effects. Such interventions could offer new hope for HCC patients, addressing the current scarcity of effective treatments. The industry is poised to explore these possibilities through continued research and development.
Emerging trends in personalized medicine further amplify the relevance of genetic markers like C1orf122, enabling treatment plans customized to individual genetic profiles. Over the next few years, from now until 2027, advancements in genomic technologies are expected to enhance the ability to leverage such markers for precise interventions. This direction signals a transformative era for HCC care, driven by data and innovation.
Global research collaborations and economic factors will also shape the trajectory of C1orf122-focused interventions. Partnerships across borders can accelerate the pace of discovery, while funding and market dynamics influence the feasibility of bringing new therapies to patients. The industry must navigate these elements strategically to ensure that promising findings translate into tangible benefits for those affected by HCC.
Reflecting on Findings and Future Steps
Looking back, the exploration of C1orf122 marked a significant stride in understanding the complex dynamics of hepatocellular carcinoma, revealing its overexpression as a harbinger of poor prognosis and its role in driving tumor progression through specific molecular pathways. The detailed analysis of its interactions and cellular impacts provided a foundation for considering it both a prognostic indicator and a therapeutic target. These insights sparked renewed interest in tackling HCC with a precision-driven mindset.
As a next step, the industry turned its attention to broader clinical validation, recognizing that diverse patient cohorts and real-world data were essential to confirm C1orf122’s relevance. Initiatives emerged to integrate animal studies and patient-derived models, aiming to bridge the gap between laboratory findings and bedside applications. This focus promised to refine the understanding of the gene’s potential across varied scenarios.
Moreover, a concerted effort unfolded to address therapeutic challenges, with research teams and pharmaceutical entities collaborating to design inhibitors that could safely target C1orf122-related pathways. The push for innovative solutions also encompassed advocacy for regulatory frameworks that balanced speed with safety, ensuring that new tools reached clinicians without compromising standards. These actionable steps laid the groundwork for a future where HCC management could be transformed through targeted, effective strategies.