Imagine a world where life-saving cancer treatments no longer require weeks of waiting for cell processing or come with a price tag in the hundreds of thousands of dollars, but instead can be administered in days at a fraction of the cost. This is the promise of in vivo CAR cell therapy, an innovative leap in immunotherapy that reprograms a patient’s own immune cells directly inside the body to fight diseases like cancer, autoimmune disorders, and even chronic infections. Unlike the traditional ex vivo CAR-T therapy, which involves extracting, genetically modifying, and reinfusing immune cells, this new approach uses advanced gene delivery systems to transform endogenous cells into disease-targeting warriors without ever leaving the patient’s system. By streamlining the process, it tackles the logistical and financial barriers that have limited access to cutting-edge treatments for many.
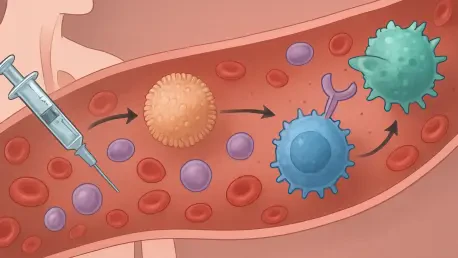
This transformative method hinges on delivering genetic instructions, known as chimeric antigen receptor (CAR) transgenes, via specialized vectors—either viral or non-viral—to instruct immune cells like T cells or macrophages to recognize and attack specific disease targets. The potential impact is staggering: preparation times could shrink from weeks to just a few days, and costs might drop to a more accessible range, potentially under $50,000 per treatment. Beyond affordability, the therapy’s adaptability to a wide range of conditions, from blood cancers to solid tumors, positions it as a cornerstone of personalized medicine. As clinical trials expand and early results show promise, the medical community is buzzing with anticipation over how this technology could reshape healthcare delivery on a global scale.
Breaking Down Barriers in Immunotherapy
Overcoming Limitations of Traditional Methods
The conventional ex vivo CAR-T therapy, while a breakthrough for treating certain blood cancers like leukemia and lymphoma, faces significant hurdles that restrict its reach. The process is labor-intensive, requiring the extraction of a patient’s T cells through apheresis, followed by genetic modification in specialized labs and reinfusion after weeks of preparation. This “vein-to-vein” timeline, often spanning 7 to 22 days, delays critical care for patients with aggressive diseases. Moreover, the financial burden is immense, with costs frequently exceeding $300,000 per treatment due to complex manufacturing and the need for dedicated facilities. Many patients, particularly in resource-limited regions, are excluded from this therapy due to geographic or economic barriers, compounded by the risks of preparatory treatments like lymphodepleting chemotherapy, which can lead to severe side effects such as infections.
Beyond logistical and financial challenges, ex vivo CAR-T therapy encounters clinical limitations that hinder its broader application. Manufacturing failures occur in up to 15% of cases due to insufficient cell quality or contamination, leaving some patients without viable treatment options. The therapy also struggles with solid tumors, where immune cells often fail to penetrate the protective barriers of the tumor microenvironment. Accessibility issues are further exacerbated for those with comorbidities who cannot tolerate invasive procedures or extended hospital stays. These persistent obstacles highlight the urgent need for an alternative approach, one that simplifies the process and extends the benefits of immunotherapy to a wider population, setting the stage for in vivo CAR therapy to address these critical gaps.
Advantages of a Streamlined Approach
In vivo CAR cell therapy represents a paradigm shift by eliminating the need for external cell manipulation, instead delivering CAR transgenes directly into a patient’s endogenous immune cells through a single infusion. This method drastically reduces preparation time to just 1-3 days, a stark contrast to the weeks required for ex vivo processes, allowing for rapid intervention in time-sensitive cases. The cost savings are equally compelling, with estimates suggesting treatments could be priced as low as $20,000 to $50,000 by cutting out expensive manufacturing steps and specialized infrastructure. By bypassing invasive procedures like apheresis and toxic regimens like lymphodepletion, the therapy minimizes patient burden and reduces the risk of associated complications, making it a more tolerable option for a broader demographic.
Additionally, the in vivo approach aligns with a pharmaceutical model similar to off-the-shelf drugs, facilitating a “ready-to-use” framework that could decentralize care delivery and make it more accessible. This streamlining opens doors to treating patients in diverse settings, including community hospitals without advanced facilities, thereby enhancing global access. The therapy’s ability to work within the body’s natural immune environment may also yield cells that are less exhausted and better equipped for sustained activity compared to lab-modified counterparts. While challenges remain in ensuring consistent efficacy across varied patient profiles, the potential to democratize access to advanced immunotherapy positions this method as a transformative force in addressing inequities in healthcare delivery.
Mechanisms and Innovations Behind the Therapy
Exploring Viral Vector Technologies
At the heart of in vivo CAR cell therapy lies the use of viral vectors, such as lentiviruses (LVs) and adeno-associated viruses (AAVs), which excel at delivering genetic material into immune cells with high efficiency. Lentiviral vectors are particularly valued for their ability to transduce both dividing and non-dividing cells, ensuring stable and long-lasting CAR expression by integrating into the host genome. However, this integration carries risks, such as insertional mutagenesis, where genes are inserted into unintended genomic locations, potentially triggering adverse effects. To mitigate this, scientists are engineering these vectors with modified surface proteins, like vesicular stomatitis virus glycoprotein (VSV-G), to enhance specificity for T cells by targeting markers such as CD3 or CD8, while eliminating natural tropism to avoid off-target cells.
Adeno-associated viruses offer a safer alternative due to their non-integrating nature, with transgenes persisting as episomes that reduce the risk of genomic disruption, making them a promising option in gene therapy. Their smaller cargo capacity, limited to about 4.7 kb, poses challenges for complex CAR constructs, and pre-existing immunity in many patients can neutralize their effectiveness. Innovations like the AAV-Ark313 variant, developed through capsid screening, have shown improved T-cell transduction without additional targeting mechanisms, achieving significant integration rates in preclinical models. Despite their promise, both LVs and AAVs can trigger immune responses, such as cytokine release syndrome (CRS), within hours of administration, necessitating rigorous safety protocols and ongoing research into reducing immunogenicity through capsid engineering and co-administration strategies.
The clinical application of viral vectors is already yielding encouraging results, with products like INT2104 targeting CD20 in B-cell malignancies demonstrating high response rates in early trials. Another example, ESO-T01, focuses on BCMA for multiple myeloma, achieving complete remission in some patients and underscoring the potential of these vectors to rival ex vivo therapies. However, manufacturing complexity and the need for strict quality controls remain significant hurdles, driving up costs and limiting scalability. As research progresses, incorporating safety switches—genetic mechanisms to deactivate CAR cells if adverse effects arise—offers a promising avenue to balance efficacy with patient safety, ensuring that viral vectors can be harnessed effectively in diverse therapeutic contexts.
Non-Viral Vectors as Emerging Alternatives
Non-viral vectors, particularly lipid nanoparticles (LNPs), are gaining momentum as a safer and more scalable option for in vivo CAR cell therapy, building on their proven success in mRNA vaccine platforms. LNPs encapsulate genetic material like mRNA or plasmid DNA within lipid structures, delivering it to immune cells with lower immunogenicity compared to viral counterparts. Their production is less complex, resembling traditional pharmaceutical manufacturing, which could significantly reduce costs and facilitate widespread distribution. However, challenges persist, including lower delivery efficiency—often below 20% in vivo—and transient expression that may require repeated dosing, raising concerns about long-term efficacy and potential immune reactions over time.
To address these limitations, advancements like targeted LNPs (tLNPs) incorporate surface ligands, such as anti-CD3 antibodies, to home in on specific immune cells, while selective organ-targeting (SORT) LNPs redirect delivery to the spleen or lymph nodes rather than the liver, a common off-target site. Products like Capstan Therapeutics’ L829-tLNP have shown success in delivering CD20 CAR mRNA to T cells in primate models, achieving B-cell depletion for autoimmune applications. Despite these strides, the transient nature of expression remains a barrier, prompting exploration into circular RNA formats that could extend therapeutic effects without frequent administrations, enhancing the practicality of non-viral systems for clinical use.
Beyond LNPs, other non-viral approaches, such as polymer nanoparticles (NPs) made from materials like poly(β-amino ester) (PBAE), offer additional flexibility by leveraging electrostatic interactions to deliver nucleic acids. Bioinspired delivery vehicles mimicking natural systems, like erythrocyte or platelet structures, improve circulation time and homing to immune-rich areas, while macroencapsulation devices, such as alginate scaffolds, enable localized CAR cell generation. These diverse tools, exemplified by studies showing leukemia clearance in mice using PBAE NPs, highlight the growing versatility of non-viral vectors. As these technologies mature, their integration into clinical pipelines, such as MT-302 targeting TROP2 in epithelial cancers, signals a future where non-viral options could rival or complement viral vectors in accessibility and impact.
Expanding Therapeutic Horizons
Targeting Diverse Immune Cells and Diseases
In vivo CAR cell therapy’s versatility extends beyond the traditional focus on T cells, embracing a broader spectrum of immune cells like macrophages, natural killer (NK) cells, and monocytes to tackle an array of diseases. While T cells are prized for their direct tumor-killing capabilities, macrophages engineered with CARs (CAR-MΦ) bring unique advantages, particularly in solid tumors where they can remodel the immunosuppressive tumor microenvironment by clearing barriers and signaling other immune responses. Preclinical studies in pancreatic cancer models have demonstrated that CAR-MΦ can disrupt protective tumor shields, enhancing overall therapeutic outcomes and suggesting a complementary role alongside T cell-based approaches in addressing complex cancers.
The scope of applications is equally expansive, reaching into autoimmune disorders where CAR-T cells can be programmed to target rogue immune components, effectively resetting the system in conditions like systemic lupus erythematosus (SLE). Products like CPTX2309, currently in early trials, aim to deplete harmful B cells directly in the body, offering a less invasive alternative to existing treatments. Additionally, in organ fibrosis—a major cause of chronic disease—CAR-T cells targeting fibroblast activation protein (FAP) have shown promise in reversing scarring in heart and liver tissues in animal models. These diverse applications underscore the therapy’s potential to address unmet needs across multiple medical fields, pushing the boundaries of what immunotherapy can achieve.
Infectious diseases, often overshadowed by cancer-focused research, are emerging as another frontier for in vivo CAR therapy, with significant potential to address pressing global health challenges. CAR-macrophages engineered to combat antibiotic-resistant bacteria have demonstrated remarkable efficacy in sepsis models, clearing infections that defy conventional treatments. This capability could position the therapy as a critical tool in acute care settings, addressing global health threats like multidrug-resistant pathogens. As research broadens to include lesser-known immune cells, such as gamma-delta T cells with unique tumor-killing properties, the adaptability of in vivo approaches continues to expand, promising tailored solutions for an ever-growing list of conditions through ongoing preclinical and clinical exploration.
Clinical Progress and Future Potential
The clinical landscape for in vivo CAR cell therapy is advancing rapidly, with over 30 trials underway, testing a range of viral and non-viral approaches across various diseases. Early results from viral vector-based therapies, such as INT2104 for B-cell malignancies, have reported impressive response rates, with some patients achieving complete remission. Similarly, ESO-T01, targeting BCMA in multiple myeloma, has shown outcomes comparable to ex vivo CAR-T therapies, validating the in vivo concept in real-world settings. These successes, while preliminary, highlight the therapy’s potential to match or even surpass traditional methods in efficacy, particularly for hematological cancers where immune targets are well-defined and accessible.
Non-viral therapies are also making strides, with LNP-based products like MT-302 targeting TROP2 in epithelial cancers entering Phase 1 trials and demonstrating encouraging safety profiles. Unlike viral vectors, which can trigger rapid immune reactions like CRS within hours, non-viral options appear to be better tolerated, though their transient expression often necessitates multiple doses to sustain therapeutic effects. Addressing persistence remains a key focus, with research into combination therapies—pairing in vivo CAR cells with cytokines like IL-7 or IL-15—showing promise in extending cell lifespan in preclinical models. As long-term data accumulate, these trials will provide critical insights into durability and safety, shaping how the therapy evolves for broader clinical adoption.
Looking ahead, the potential to integrate in vivo CAR therapy with cutting-edge tools like CRISPR offers a pathway to even greater precision, allowing for targeted genetic modifications that enhance safety and effectiveness. The therapy’s adaptability to new disease targets, from novel cancer markers to viral proteins, ensures it remains relevant as medical challenges shift. However, scaling these innovations requires overcoming manufacturing and regulatory hurdles, particularly for viral vectors that demand stringent quality controls. Collaborative efforts across biology, engineering, and clinical fields are essential to refine vector design, standardize dosing, and expand access, paving the way for in vivo CAR therapy to transition from experimental to mainstream care in the coming years.
Addressing Challenges and Shaping the Future
Navigating Safety and Efficacy Concerns
Safety remains a paramount concern in the development of in vivo CAR cell therapy, particularly with viral vectors that can provoke severe immune responses shortly after administration. Cytokine release syndrome (CRS), a potentially life-threatening reaction characterized by fever and organ dysfunction, has been observed in early trials, necessitating proactive interventions like tocilizumab to manage symptoms. To mitigate such risks, researchers are embedding safety switches—genetic mechanisms that allow CAR cells to be deactivated if adverse effects emerge—into vector designs, providing clinicians with greater control over the therapy’s course. These advancements aim to balance the potent efficacy of viral delivery with the imperative of patient well-being, ensuring safer therapeutic outcomes.
Non-viral vectors, while generally less immunogenic, face their own set of challenges related to efficacy, as their transient expression often fails to sustain long-term CAR cell activity compared to ex vivo counterparts. Repeated dosing, while a potential solution, raises concerns about cumulative immune reactions and treatment costs over time. Innovations such as circular RNA, which offers prolonged expression without genomic integration, are being explored to enhance durability without compromising safety. Additionally, real-time monitoring during clinical trials helps adjust dosing dynamically based on individual responses, addressing variability in transduction efficiency across patients. As these strategies evolve, they promise to refine the risk-benefit profile of non-viral approaches, making them viable for widespread use.
The complexity of immune responses in vivo adds another layer of difficulty, as not all patients react uniformly to vector delivery or CAR expression, and factors like pre-existing immunity to viral vectors or differing immune cell compositions can influence outcomes. This necessitates personalized approaches to dosing and vector selection to ensure effective treatment. Ongoing studies are leveraging biomarkers to predict patient responses, aiming to tailor therapies to individual profiles for optimal results. Meanwhile, long-term follow-up in trials is critical to detect delayed side effects, such as genotoxicity from viral integration, ensuring that safety protocols keep pace with the therapy’s rapid advancement. These efforts collectively strive to build trust in the technology, addressing both immediate and future concerns with rigorous scientific inquiry.
Manufacturing and Regulatory Pathways
Manufacturing in vivo CAR cell therapy presents distinct challenges, particularly for viral vectors that require intricate production processes under good manufacturing practice (GMP) standards to ensure purity and consistency. The complexity of cultivating viral particles, coupled with the need for stringent quality controls to prevent contamination or batch variability, drives up costs and limits scalability, posing a barrier to widespread adoption. Efforts to automate production and develop closed-system bioreactors are underway to streamline processes, reduce expenses, and meet the growing demand for therapies as clinical trials expand. These innovations aim to make viral vector-based treatments more accessible while maintaining the high standards necessary for patient safety.
Non-viral vectors, such as lipid nanoparticles, offer a more straightforward manufacturing pathway, drawing on established pharmaceutical models that resemble vaccine production. Their scalability is a significant advantage, as seen in the rapid rollout of mRNA vaccines, allowing for cost-effective mass production that could lower therapy prices significantly. However, challenges remain in optimizing formulations to improve delivery efficiency and expression duration, requiring investment in next-generation materials like ionizable lipids for better cellular uptake. As non-viral systems advance, harmonizing production standards across different platforms will be essential to ensure consistency and reliability, facilitating their integration into routine clinical practice without compromising quality.
Regulatory frameworks are adapting to the unique nature of in vivo CAR therapies, which differ from traditional drugs or even ex vivo cell therapies due to their direct genetic modification within the body. Agencies like the FDA are collaborating with researchers to define clear approval pathways, emphasizing long-term safety data to address risks like delayed toxicities or off-target effects. Establishing standardized endpoints for efficacy—whether tumor shrinkage in cancer or immune balance in autoimmune conditions—remains a priority to evaluate success across diverse indications. Additionally, global harmonization of regulations could accelerate access by aligning trial requirements across regions, ensuring that breakthroughs reach patients worldwide without unnecessary delays driven by disparate oversight.
Economic and ethical considerations also intersect with regulatory and manufacturing challenges, as stakeholders grapple with how to price therapies affordably while covering development costs. Value-based pricing models, where payment reflects patient outcomes, are being explored to balance accessibility with innovation incentives. Meanwhile, transparent communication about the therapy’s risks and benefits is vital to maintain public trust, especially given the novelty of in vivo genetic modifications. As interdisciplinary teams of scientists, manufacturers, and policymakers collaborate, their combined efforts aim to navigate these multifaceted hurdles, setting a foundation for the therapy to become a sustainable and equitable component of modern medicine.
Envisioning Broader Impacts and Next Steps
Reflecting on the strides made, the journey of in vivo CAR cell therapy revealed a remarkable evolution from experimental concepts to tangible clinical outcomes that reshaped patient lives. Early trials demonstrated that therapies like ESO-T01 achieved remission in multiple myeloma cases where hope had dwindled, while non-viral approaches like MT-302 offered safer profiles for solid tumor patients. Preclinical successes in diverse areas, from reversing organ fibrosis to combating resistant infections, underscored the therapy’s vast potential. These milestones, accomplished through persistent innovation, highlighted how a once-niche idea matured into a viable alternative to conventional treatments, despite hurdles in safety and scalability that demanded careful resolution.
Looking to actionable next steps, prioritizing cross-disciplinary collaboration stands as a critical pathway to refine this technology further and ensure its success in the long term. Combining expertise in synthetic biology for smarter vector designs, nanotechnology for enhanced delivery, and clinical science for optimized trial protocols can accelerate progress. Investment in scalable manufacturing, especially for non-viral systems, should be ramped up to drive costs down, while regulatory bodies must streamline approval processes without sacrificing rigor. Expanding trial access to underrepresented regions could ensure equitable benefits, supported by global data-sharing initiatives to inform real-world efficacy. Ultimately, fostering a dialogue between patients, providers, and researchers will help tailor in vivo CAR therapy into a cornerstone of future healthcare, addressing both current challenges and emerging needs with precision and compassion.