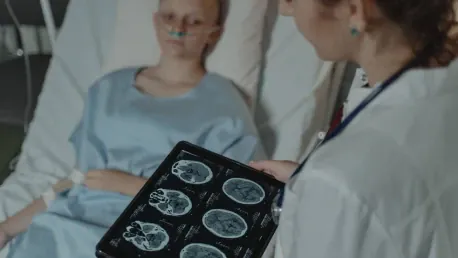
The relationship between social risks and routine cancer screenings signifies a complex and pressing public health issue, particularly regarding how housing instability or food insecurity among patients significantly hinders essential cancer preventive care. A new study conducted by researchers at the University of California San Diego, in collaboration with several other institutions, delves into this issue and brings to light the intricate pathways through which social risks negatively impact cancer prevention efforts, emphasizing the necessity for tailored interventions to confront these barriers effectively.
The Role of Social Risks in Cancer Screening
Identifying Social Risks as Barriers
A key theme revealed by the study is that social risks constitute critical barriers that significantly decrease the chances of patients receiving and completing orders for cancer screenings, despite relatively higher rates of primary care visits. Patients struggling with social risks like food insecurity, housing instability, and transportation insecurity exhibit a lower probability of undergoing routine screenings for cervical, colorectal, and breast cancers. This discrepancy suggests that access to healthcare is not the main issue; instead, social risks create substantial obstacles to preventive health measures.
Lead author Matthew P. Banegas, Ph.D., M.P.H., and his team leveraged electronic health record data from OCHIN, a nonprofit health IT consultancy serving community health centers and rural hospitals. Their research skimmed through data from 186 community-based healthcare organizations (CBHCOs) across 13 states, focusing on underserved populations such as low-income, rural, and immigrant groups. Despite the vital role CBHCOs play in providing necessary care at minimal or no cost, the patients they serve continue to bear a heavier burden of social risks compared to the general U.S. population.
Impact on Specific Cancer Screenings
The study delineated that social health drivers profoundly influence patients’ capabilities to receive necessary cancer screenings, and these effects vary according to specific risks and cancer types. For instance, food insecurity correlates with a lower probability of receiving orders for all three types of cancer screenings. Cervical cancer screenings are particularly less frequent for patients confronting transportation insecurity. Furthermore, the completion rates for ordered cervical and colorectal cancer screenings are lower among patients dealing with food insecurity, whereas those with transportation insecurity show decreased completion rates for colorectal cancer screenings. Interestingly, breast cancer screening completion rates did not significantly differ between patients with or without social risks.
The Influence of Social Determinants on Health Outcomes
Urgency of Immediate Needs
One of the more prominent trends emphasized in the study is the critical impact of social determinants on health outcomes. Researchers suggest that the acute nature of food insecurity might divert the focus of primary care visits from preventive care to more pressing health risks. This sense of urgency can result in delays in both ordering and completing cancer screenings. Logistical challenges associated with housing instability and transportation insecurity might also hinder patients’ abilities to adhere to additional appointments or procedures needed for certain screenings, such as colonoscopies or Pap tests. In contrast, mammograms are easier to complete, partly due to supportive outreach programs like mobile mammography clinics.
Policy Changes and Health Equity
The study also sheds light on recent policy changes aimed at addressing social determinants of health, with particular focus on the Centers for Medicare and Medicaid Services (CMS) mandate. This mandate requires health systems to screen patients for social risks and connect those with unmet needs to relevant services. This policy shift represents a significant step toward health equity, acknowledging the critical necessity of a holistic healthcare approach that proactively addresses social risks in clinical settings.
Future Directions and Recommendations
Continued Research and Strategy Development
Looking ahead, the study’s authors advocate for further research into the pathways linking social risks and health outcomes, as well as for the development of effective strategies to manage these challenges. Investing in prevention and early intervention allows the healthcare system to not only curb overall healthcare costs but also significantly enhance patient health outcomes. The collaborative nature of this research underscores the importance of a multidisciplinary approach in tackling complex health issues, involving experts from institutions like the University of California San Diego, Oregon Health & Science University, and Massachusetts General Hospital.
Practical Solutions for Healthcare Providers
The link between social risks and routine cancer screenings points to a complex and urgent public health issue, especially considering how housing instability and food insecurity among patients considerably obstruct needed cancer preventive care. A recent study by researchers at the University of California San Diego, alongside several other institutions, investigates this concern deeply. The research uncovers the detailed ways in which these social risks negatively affect cancer prevention efforts. It reveals that patients facing homelessness or lack of proper nutrition are less likely to receive regular screenings, which are essential for early detection and treatment. Consequently, these individuals are at a higher risk of advanced cancer stages when finally diagnosed. The study underscores the importance of creating and implementing targeted interventions to effectively address these obstacles. Tailored solutions are essential to ensure that preventive cancer care becomes accessible to everyone, regardless of their social circumstances. The research calls for a combined effort to mitigate these risks and enhance public health outcomes.