We’re joined today by Ivan Kairatov, a leading biopharma expert whose work is at the forefront of understanding our complex relationship with the microscopic world inside us. His team’s recent discoveries are reshaping how we view the common fungus Candida albicans—not just as a potential threat, but as a finely balanced resident of our bodies. This conversation will explore the elegant, and sometimes precarious, dance between this fungus and our immune system. We’ll delve into how a fungal toxin can be both a tool for peaceful coexistence and a trigger for disease, the critical role of an immune signal known as Interleukin 17 in keeping the fungus in check, and a fascinating defense strategy where our body starves the fungus of a key nutrient. Ultimately, this research provides a new lens through which to view infections and the side effects of modern immunotherapies.
Your research describes the fungal toxin candidalysin as a “door opener” in small amounts but a trigger for severe inflammation in large amounts. Could you walk us through the molecular process of how the fungus regulates this toxin to maintain its “handbrake on” state in a healthy host?
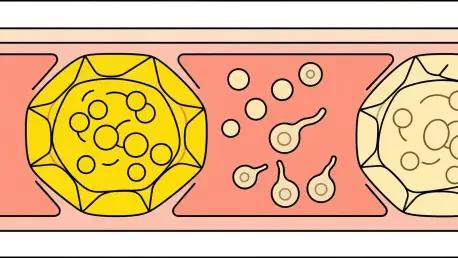
That’s an excellent way to put it. The fungus truly operates with its “handbrake on.” It’s a matter of survival and strategy. In our research, we observed that Candida albicans needs a tiny amount of candidalysin to gain a foothold. Think of the toxin as a key. The fungus produces just enough to gently “unlock” the surface of the oral mucosa, allowing it to anchor itself without setting off any alarms. This minimal expression is crucial for it to exist as a harmless colonizer. The moment it ramps up production and releases large quantities of the toxin, it’s like shouting in a library. The immune system, which was previously ignoring it, immediately registers a direct attack on host cells and responds with overwhelming force, triggering severe inflammation. So, the fungus itself maintains this delicate balance, knowing that overstepping will be “punished” by a swift and potent immune retaliation.
You identify Interleukin 17 as a “gatekeeper” that controls Candida albicans. When this gatekeeper is lost, what is the specific cascade of events you observed in our mouse models that leads from fungal changes to the development of chronic disease and tissue damage?
The “gatekeeper” analogy is perfect because its absence truly unleashes chaos. In our mouse models where the Interleukin 17 pathway was compromised, the first thing we saw was a dramatic, uncontrolled explosion in the fungal population. With the gatekeeper gone, the fungus was no longer restricted. This overgrowth was immediately followed by a profound shift in its very form; it began to grow in its filamentous, pathogenic state, forming invasive hyphae that can burrow into tissue. This transformation was coupled with a massive spike in candidalysin production, the toxin we just discussed. This creates a destructive feedback loop: the invasive filaments cause physical damage, while the high toxin levels poison the surrounding cells, leading to significant tissue destruction and the chronic, painful inflammation characteristic of oral thrush.
The study highlights ‘nutritional immunity’ where IL-17 sequesters zinc from the fungus. Can you elaborate on the cellular mechanisms behind this process? For instance, what measurable changes in zinc levels or fungal hyphae formation did you record when this immune pathway was active versus inactive?
‘Nutritional immunity’ is one of the most elegant defense mechanisms we’ve observed. It’s not about fighting the fungus directly, but about starving it of a critical resource. IL-17 essentially sends a signal to the host’s own cells in the mucosa, telling them to lock away all available zinc, making it inaccessible to the fungus. In our experiments where the IL-17 pathway was active, the impact was visually and measurably stark. The fungus simply couldn’t get the zinc it needs to build its dangerous tools. We observed that the formation of invasive hyphae was dramatically inhibited—the yeast cells largely remained in their round, less harmful form. Furthermore, the production of candidalysin plummeted. Conversely, in the models lacking IL-17, the fungus had unfettered access to zinc. It was like a construction site that suddenly received a massive supply of steel—the fungus rapidly built its invasive structures and churned out the toxin, leading to full-blown infection.
Given that immunotherapies blocking the IL-17 pathway can cause thrush, how might your findings on zinc sequestration influence future clinical strategies? Can you give an anecdote or a hypothetical example of how this knowledge could change how we manage these side effects in patients?
This is where our research has profound clinical implications. We know these IL-17 inhibitors are incredibly effective for conditions like psoriasis, but a fraction of patients pay the price with recurrent candidiasis. Right now, we just treat the thrush with antifungals when it appears. But imagine a different approach. A patient on one of these therapies starts developing thrush. Instead of just prescribing another round of fluconazole, we could use our knowledge of nutritional immunity. We might develop a therapeutic mouthwash or a topical gel containing a compound that helps the oral cells sequester zinc more effectively, essentially restoring the local defense mechanism that the systemic drug has suppressed. This way, we could potentially prevent the thrush from ever starting, without interfering with the beneficial effects of the immunotherapy on the patient’s primary disease. It’s about re-establishing the local balance, fighting smarter, not harder.
What is your forecast for developing new therapies that target these host-fungus interactions, especially given the rise of immunotherapies and concerns about antifungal resistance?
My forecast is one of cautious optimism, leaning toward a paradigm shift in treatment. For decades, our main strategy has been to find new ways to kill the fungus, which inevitably leads to an arms race and the rise of antifungal resistance. I believe the future lies in modulation, not annihilation. Instead of trying to eradicate Candida, which is a natural part of our microbiome, we will develop therapies that keep it in its harmless, commensal state. We could design drugs that specifically block the production of candidalysin or enhance the host’s zinc sequestration pathway. This approach is far more sustainable. It’s about reinforcing our body’s natural diplomacy with its microbial residents, ensuring they remain peaceful neighbors rather than becoming dangerous invaders. This becomes especially critical as our population ages and the use of immunosuppressive therapies continues to grow.