Glioblastoma, recognized as the most aggressive and common form of brain cancer, especially in its IDH wild-type variant, remains a daunting challenge with survival rates often limited to about a year despite intensive treatments like surgery, radiotherapy, and chemotherapy. A groundbreaking study from Juntendo University, led by Associate Professor Akifumi Hagiwara and published on October 11 in a leading journal, offers a compelling new perspective on this deadly disease. The research shifts the focus from the tumor itself to the brain’s broader internal environment, specifically its fluid dynamics. This revelation suggests that survival outcomes may be influenced by how effectively the brain manages waste clearance and fluid circulation, even in areas far from the tumor. Such a perspective not only challenges conventional approaches but also sparks hope for innovative strategies that could redefine the fight against this devastating condition, opening pathways to improved patient prognosis.
Uncovering the Glymphatic System’s Hidden Influence
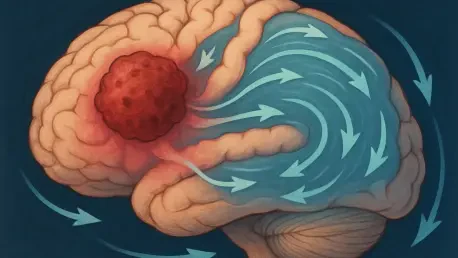
The brain’s glymphatic system, a vital network responsible for clearing waste and circulating fluids, emerges as a key factor in glioblastoma survival according to this recent study. Unlike past research that focused on the tumor’s immediate surroundings, this investigation reveals that disruptions in fluid dynamics, particularly in the contralateral hemisphere—the side of the brain opposite the tumor—have a significant impact on patient outcomes. These distant disturbances indicate that glioblastoma causes a systemic imbalance, leading to toxic accumulation and increased neural damage beyond the tumor’s location. This finding redefines the disease as more than just a localized growth, suggesting that the brain’s overall environment plays an equally important role in determining how long patients might survive. It’s a shift that compels medical professionals to consider the broader implications of brain health when addressing this aggressive cancer.
Further exploration into the glymphatic system’s dysfunction highlights how such imbalances worsen the challenges faced by glioblastoma patients. The research points to a correlation between impaired fluid movement and the buildup of harmful substances, which can inflame brain tissue and speed up disease progression. Even areas of the brain that appear unaffected on standard scans show signs of disrupted circulation, painting a picture of a condition that affects the entire neural landscape. This systemic effect underscores the limitations of traditional treatments that focus solely on tumor removal or containment. By identifying the glymphatic system as a key player, the study lays the groundwork for rethinking therapeutic approaches, potentially integrating methods to support fluid balance as a complementary strategy. This broader understanding could be crucial in crafting more effective interventions for those battling this relentless form of cancer.
Advanced Imaging as a Window to Prognosis
To uncover these critical insights, the research team used advanced MRI techniques such as Diffusion Tensor Imaging along the Perivascular Space (DTI-ALPS) and Free Water (FW) imaging. DTI-ALPS measures how easily water molecules travel along channels near blood vessels, providing a gauge of fluid movement efficiency, while FW imaging quantifies the amount of fluid trapped between brain cells, indicating accumulation levels. The results were striking: patients with a lower ALPS index, signifying slower water movement, and higher FW levels, showing greater fluid buildup, consistently faced shorter survival times, even in brain regions distant from the tumor. This evidence of widespread dysfunction suggests that glioblastoma’s impact extends far beyond its physical boundaries, affecting the brain’s ability to maintain a healthy internal environment through effective waste clearance.
These imaging tools offer more than just diagnostic insights; they provide a non-invasive way to predict patient outcomes with remarkable precision. By analyzing fluid dynamics through such advanced methods, clinicians can identify individuals at higher risk early in their treatment journey, allowing for tailored interventions that address specific vulnerabilities. This approach marks a significant departure from standardized protocols, paving the way for personalized care plans that consider the unique state of each patient’s brain environment. For instance, those showing severe glymphatic impairment might benefit from intensified therapies or experimental treatments aimed at restoring fluid circulation. The potential of these MRI-based assessments to guide clinical decisions represents a transformative step toward improving survival rates and enhancing the quality of life for glioblastoma patients facing an otherwise grim prognosis.
Paving the Way for Innovative Treatments
Beyond prognosis, the study sparks intriguing possibilities for novel therapeutic strategies that target the brain’s fluid dynamics. Enhancing glymphatic function through lifestyle adjustments like optimizing sleep patterns, which are known to support waste clearance during rest, or reducing inflammation through targeted medications, could offer new ways to improve patient outcomes. Additionally, exploring the role of specific water channels in the brain, known as aquaporins, might lead to interventions that directly improve fluid movement. While these concepts are still in exploratory stages, they suggest a future where supporting the brain’s natural cleansing mechanisms could complement conventional treatments such as surgery and chemotherapy, potentially extending survival and lessening the harsh effects of the disease.
The prospect of integrating such innovative therapies into standard care protocols is both promising and challenging. Developing treatments that enhance glymphatic function requires further research to validate their effectiveness and safety, but the potential rewards are substantial. Imagine a scenario where a combination of tumor-focused therapies and fluid balance interventions work together to combat glioblastoma from multiple angles. This dual approach could not only slow disease progression but also ease some of the debilitating symptoms caused by toxic buildup in the brain. As science advances, these ideas might evolve into concrete solutions, offering renewed hope to patients and families grappling with a diagnosis that has long been associated with limited options. The journey toward these advancements, though complex, signifies a critical shift toward more holistic and effective cancer care.
Redefining Brain Health in Neurological Diseases
This research extends its relevance beyond glioblastoma, aligning with a growing recognition of the brain’s internal environment as a fundamental factor in various neurological conditions. Disorders like Alzheimer’s disease, where impaired waste clearance also contributes to progression, share striking similarities with the findings related to brain fluid dynamics in cancer. This overlap suggests that lessons learned from studying glioblastoma could inform broader strategies for managing other brain-related ailments, emphasizing the interconnectedness of neural health. By reframing glioblastoma as a condition of systemic dysfunction rather than merely uncontrolled cell growth, the study advocates for a comprehensive approach that prioritizes the brain’s overall balance alongside targeted tumor treatments.
Reflecting on the past impact of such revelations, it becomes clear that this shift in perspective prompted a reevaluation of how neurological diseases were approached in clinical settings. The recognition of fluid dynamics as a critical determinant of health encouraged researchers and practitioners to explore integrative methods that addressed both specific pathologies and the brain’s wider environment. Looking back, the push for holistic strategies inspired subsequent studies to investigate similar mechanisms in other conditions, fostering a deeper understanding of neural resilience. Moving forward, the medical community can build on these insights by investing in research to validate and refine therapies that restore fluid balance, ensuring that future patients benefit from a more nuanced and effective framework for combating devastating brain disorders.