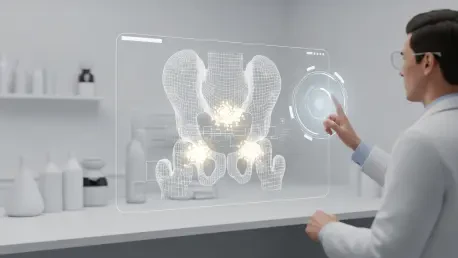
For men who have undergone surgery to remove their prostate, a subsequent rise in a key blood marker often signals the cancer’s return, plunging them into a period of clinical uncertainty where the next steps have historically been guided more by protocol than precision. This research summary explores a transformative shift in this paradigm, detailing how an advanced imaging technique known as prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) is enabling a move toward highly personalized, anatomy-guided salvage therapy. The central challenge addressed is the transition from standardized treatment for everyone to a tailored approach that targets the cancer exactly where it is, promising better outcomes with fewer side effects.
This investigation delves into how PSMA PET/CT imaging can not only predict a patient’s progression-free survival but also guide individualized treatment plans for those experiencing a biochemical recurrence after radical prostatectomy. By offering a clear map of recurrent disease, these scans provide the crucial information needed to refine and personalize secondary therapies, a pivotal step forward in the ongoing fight against prostate cancer.
The Shift Toward Personalized Anatomy-Guided Salvage Therapy
The journey for a prostate cancer patient does not always end with surgery. For a significant number of men, a rise in prostate-specific antigen (PSA) levels after a radical prostatectomy signals a biochemical recurrence, a frustrating and often frightening development. For years, the inability to precisely locate the source of this recurrence created a major clinical dilemma, compelling physicians to rely on standardized salvage treatments, such as broad-field radiation to the pelvis, which were applied without knowing the exact location or extent of the disease. This “one-size-fits-all” model often resulted in either overtreatment, exposing patients to unnecessary toxicity, or undertreatment, failing to control the cancer’s spread.
This research addresses the urgent need to move beyond these generalized protocols. It is founded on the principle that effective treatment requires knowing the enemy’s location. The study explores how the anatomical information provided by PSMA PET/CT scans can be leveraged to craft individualized salvage therapy plans. Instead of treating all patients with biochemical recurrence the same way, this new approach allows clinicians to tailor the intensity and scope of treatment—from highly focused radiation to systemic therapies—directly to the disease burden revealed by the scan. This represents a fundamental shift toward a more precise, effective, and patient-centric standard of care.
The Challenge of Biochemical Recurrence and the Advent of PSMA Imaging
Following the complete surgical removal of the prostate, a detectable or rising PSA level is a clear indicator that prostate cancer cells remain or have returned somewhere in the body. This situation, known as biochemical recurrence, presents a significant clinical challenge. Historically, conventional imaging techniques like CT and bone scans lacked the sensitivity to detect small-volume recurrent disease, especially at the very low PSA levels where intervention is most effective. This “imaging blindness” left clinicians and patients in a difficult position, forced to make critical treatment decisions based on statistical probabilities rather than direct evidence.
The development of highly sensitive PSMA PET/CT imaging has revolutionized this landscape. This advanced molecular imaging technique targets a protein found in high concentrations on the surface of prostate cancer cells, allowing it to “light up” even microscopic deposits of cancer anywhere in the body. For the first time, physicians can visualize the exact location and extent of recurrent disease with remarkable accuracy. This breakthrough provides the missing piece of the puzzle, transforming the management of biochemical recurrence from a standardized guessing game into a precise, targeted intervention. This research is therefore crucial for validating how this powerful tool can be used to improve patient outcomes and minimize the collateral damage of unnecessary treatment.
Research Methodology Findings and Implications
Methodology
Researchers at the University of California Los Angeles (UCLA) Jonsson Comprehensive Cancer Center conducted a detailed retrospective analysis to investigate the clinical utility of PSMA PET/CT scans in the post-prostatectomy setting. The study included 113 prostate cancer patients who had all undergone a radical prostatectomy and subsequently experienced a biochemical recurrence. A key aspect of the methodology was the uniform staging of all participants using PSMA PET/CT imaging, which provided a precise anatomical map of recurrent disease for each individual.
The core of the analysis focused on evaluating the correlation between the findings on these scans—specifically, the location and extent of the cancer—and the patients’ long-term progression-free survival following salvage therapy. By examining how different patterns of recurrence responded to various treatment strategies, the researchers aimed to establish an evidence-based framework for using these advanced imaging results to guide more effective and personalized therapeutic decisions.
Findings
The study’s results established a direct and powerful link between the patterns of disease identified on PSMA PET/CT scans and the efficacy of subsequent treatments. The anatomical information gleaned from the scans proved to be a more reliable predictor of patient response than traditional biomarkers like the absolute PSA level. Based on the scan findings, patients were successfully stratified into three distinct groups, each benefiting from a different therapeutic approach.
For patients with no visible signs of disease on their scans, the prognosis was excellent, and localized radiation to the prostate bed alone was sufficient. In this group, more extensive treatments like whole-pelvis radiotherapy offered no additional benefit and would have only increased the risk of side effects. In contrast, for patients with visible, localized disease confined to the pelvic region, a broader field of treatment encompassing the whole pelvis significantly improved progression-free survival. Finally, in cases where the cancer had spread to pelvic lymph nodes or distant sites, the study confirmed that radiotherapy alone was insufficient. The addition of systemic androgen deprivation therapy (ADT) was necessary to achieve better long-term outcomes for these patients.
Implications
The implications of this research are profound, signaling a necessary evolution in the standard of care for men with recurrent prostate cancer. The findings provide strong evidence that PSMA PET/CT scans should be integrated as a routine diagnostic tool for any patient being considered for salvage therapy after surgery. The detailed anatomical information provided by the scan frequently leads to a change in the recommended treatment plan, shifting it from a standardized protocol to a strategy tailored to the individual’s specific disease pattern.
This paradigm shift enables a more intelligent application of therapy, which has a dual benefit. First, it enhances treatment efficacy by ensuring that the selected therapy is appropriate for the cancer’s spread—whether it requires localized radiation, regional treatment, or systemic therapy. Second, it dramatically improves patient safety and quality of life by preventing the toxicities associated with unnecessary or ineffective treatments. By accurately identifying who needs more aggressive therapy and, just as importantly, who does not, clinicians can maximize benefits while minimizing harm.
Reflection and Future Directions
Reflection
This study successfully validates a core principle of modern oncology: the ability to see the cancer is fundamental to treating it effectively. A key reflection from the research is the clear superiority of advanced anatomical imaging over traditional clinical biomarkers in predicting long-term outcomes and guiding therapy in the salvage setting. The PSMA PET/CT scan provides a level of detail that transforms treatment planning, allowing clinicians to match the therapeutic strategy directly to the patient’s disease distribution.
The evidence reinforces the necessity of abandoning the “one-size-fits-all” model that has long dominated the management of biochemical recurrence. Instead of treating the PSA level, clinicians can now treat the cancer itself, wherever it may be hiding. This approach not only makes intuitive sense but is now supported by robust clinical data, marking a significant step forward in the quest for precision medicine in prostate cancer care.
Future Directions
While this retrospective analysis provides compelling evidence for the value of PSMA PET/CT imaging, the logical next step is to confirm these findings through prospective, randomized clinical trials. Future research should be designed to formally test these anatomy-guided treatment strategies against current standard-of-care approaches. Such trials are essential for cementing these findings into new, evidence-based clinical practice guidelines.
Looking ahead, further studies could also explore the role of PSMA imaging in other stages of prostate cancer, including initial diagnosis and the monitoring of treatment response. The ultimate goal is to fully integrate this powerful imaging tool into the standard of care for managing prostate cancer, ensuring that every patient receives the most effective and personalized treatment possible from the outset. This will require continued collaboration and research to refine protocols and establish the optimal use of this transformative technology.
A New Era of Precision in Prostate Cancer Management
The findings from this research heralded a pivotal moment in the management of recurrent prostate cancer. It was demonstrated that PSMA PET/CT scans are not merely an incremental improvement but a truly transformative tool that empowers clinicians to personalize therapy with unprecedented accuracy. By providing a clear anatomical roadmap of recurrent disease, these scans enabled the selection of the most effective and least toxic treatments for each individual patient.
This shift toward anatomy-guided care ultimately improved progression-free survival and redefined the approach to salvage therapy after prostate surgery. The ability to tailor treatment based on precise visual evidence marked the beginning of a new, more hopeful era, one in which prostate cancer management is driven by precision, efficacy, and a profound respect for patient quality of life.