The intricate relationship between our gut microbiota and the risk of developing colon cancer has captivated scientific interest recently, revealing new layers of complexity in how our body’s internal systems interact. Researchers at the University of Wisconsin-Madison have discovered that microbial bile acids in the gut have contrasting effects on the risk of developing colon cancer. These groundbreaking findings indicate that the gut microbiome’s influence on colon cancer risk is mediated through the modification of bile acids, substances produced by the liver to break down fats. This study highlights how these microbially-modified bile acids affect the farnesoid X receptor (FXR), a protein that plays a critical role in maintaining gut health. FXR not only regulates bile acid production in the liver but also responds distinctively to bile acids altered by gut microbes. This dual effect of modified bile acids on FXR is significant, as it directly impacts the development of tumors in the intestines, suggesting that some bile acids may slow down cancer growth while others may hasten tumor development.
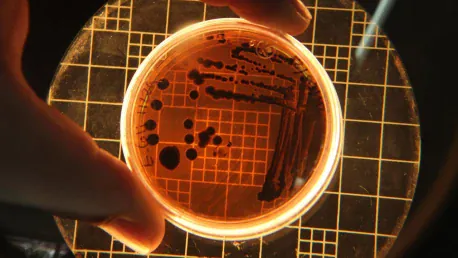
The research, conducted across various models including mouse models of colon cancer and organoids derived from human colon cancer patients, is the first to link specific microbial bile acids to either the promotion or prevention of colorectal cancer. These findings underscore the complex interactions within our gut that significantly affect our overall health. A detailed understanding of these mechanisms provides a potential pathway for improving early detection and developing targeted therapies for colorectal cancer, which could benefit millions of people worldwide. This study opens new doors to exploring how gut microbiota can profoundly impact not just gut health but our susceptibility to serious diseases like colon cancer.
Microbial Modification of Bile Acids
At the root of these findings is the process by which microbes in the gut modify bile acids produced by the liver. Bile acids are crucial for the digestion and absorption of dietary fats, initially synthesized in the liver and then modified as they travel through the intestines. Gut microbes play an essential role in this modification process, resulting in a variety of bile acids that can either enhance or inhibit the function of the farnesoid X receptor (FXR). FXR is a nuclear receptor that regulates bile acid synthesis in the liver and maintains gut homeostasis by controlling the expression of genes involved in bile acid metabolism, inflammation, and tumor suppression.
The dual nature of how modified bile acids affect FXR is central to understanding their impact on colon cancer risk. Some microbial bile acids are found to enhance FXR function, which is linked to the suppression of tumor growth. Others, however, were observed to inhibit FXR, thereby promoting the development of intestinal tumors. This discovery suggests that the specific composition of gut microbiota, and consequently the types of bile acids produced, can influence the likelihood of developing colon cancer. The study’s consistency across different models, particularly mouse models of colon cancer and human-derived organoids, reinforces the robustness of these findings.
FXR and Tumor Development
FXR’s involvement in tumor growth offers a key insight into the development and progression of colorectal cancer. FXR plays a complex role within the gut, influencing various pathways that can either suppress or promote cancer development. When FXR function is enhanced by certain microbial bile acids, it supports gut health, mitigates inflammation, and reduces tumor growth. On the other hand, when FXR is inhibited by other bile acids, it can lead to increased cancer cell proliferation and tumor development. This duality highlights the importance of maintaining a balanced gut microbiota to ensure the production of bile acids that favor FXR function, thus reducing cancer risk.
The implications of these findings extend beyond basic research, offering potential applications in clinical settings. By understanding how different gut microbes influence bile acid composition and FXR activity, healthcare providers can explore new strategies for early detection of colorectal cancer. Additionally, this knowledge paves the way for developing targeted therapies that modulate bile acid composition or FXR activity to prevent or treat colorectal cancer. Postdoctoral researcher Xingchen Dong, the lead author of the study, emphasized the significance of these results, noting that they represent a major advancement in the field of gut microbiome research and its connection to cancer.
Future Research and Potential Therapies
Scientists have recently uncovered layers of complexity concerning how our gut microbiota influences colon cancer risk. Researchers from the University of Wisconsin-Madison found that microbial bile acids in the gut can both increase and decrease colon cancer risk, depending on their interaction with the farnesoid X receptor (FXR). This receptor is critical for gut health as it regulates bile acid production in the liver and responds to bile acids modified by gut microbes. This study reveals how some modified bile acids can slow cancer progression, while others may promote tumor growth. The research utilized various models, including mouse models and human-derived organoids, to establish the connection between specific microbial bile acids and colorectal cancer outcomes.
These pivotal findings highlight the need to understand the complex gut interactions that influence our health. The research offers hope for improving early detection and developing targeted treatments for colorectal cancer. The study opens new avenues for exploring how our gut microbiota impacts our overall health and susceptibility to severe diseases like colon cancer, potentially benefiting people worldwide.