The startling reality that over 30% of adults may carry dangerous fat deposits deep within their abdomen or liver, even without visible signs of obesity, has sparked intense discussion in the medical community. This hidden fat, often undetectable through traditional measures like body mass index (BMI), poses a significant threat to cardiovascular health by contributing to artery damage. What does this mean for heart disease prevention, and how are experts responding to this silent epidemic? This roundup gathers diverse opinions, research insights, and practical tips from various health professionals and studies to uncover the risks of visceral and hepatic fat, challenge outdated assessment methods, and explore innovative solutions for better health outcomes.
Exploring the Dangers of Hidden Fat from Multiple Perspectives
Visceral Fat: A Universal Threat to Artery Health
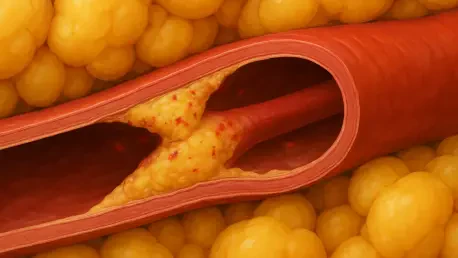
Research across large population studies in North America and Europe consistently points to visceral fat—stored around internal organs—as a critical driver of carotid artery plaque buildup and wall thickening. Data from cohorts of over 33,000 adults reveal a direct correlation between these fat deposits and heightened risks of strokes and heart attacks, regardless of external body weight. Many cardiologists emphasize that this internal fat often escapes detection in standard checkups, making it a stealthy yet potent hazard.
Beyond the numbers, metabolic health specialists highlight inflammation as a primary mechanism through which visceral fat damages arteries. Even when cholesterol or blood pressure levels are managed, this inflammatory response persists, catching many patients and doctors off guard. The consensus among these experts is that relying solely on visible indicators of health can lead to missed opportunities for early intervention.
A contrasting view from some public health advocates suggests that while the danger is real, the focus should also include lifestyle factors like diet and stress, which can exacerbate fat accumulation. They argue for a broader educational push to inform people about how daily habits contribute to this hidden risk, complementing clinical findings with actionable prevention strategies.
Hepatic Fat: An Overlooked Contributor to Cardiovascular Risk
Turning to hepatic fat, or fat stored in the liver, opinions vary on its impact compared to visceral fat, though most researchers agree it plays a notable role in artery harm. Studies involving diverse groups show that while the link is less pronounced, liver fat still contributes to cardiovascular strain, often without any outward symptoms. Nutritionists point out that this accumulation frequently results from diets high in processed sugars, yet it remains under-discussed in routine medical assessments.
Some endocrinologists stress the challenge of detecting hepatic fat without specialized imaging, noting that many patients remain unaware of their risk until significant damage occurs. They advocate for increased access to diagnostic tools to catch this issue early, especially in middle-aged populations where prevalence tends to rise. Their perspective underscores a gap in current healthcare practices that needs urgent attention.
On the other hand, a smaller group of general practitioners argues that while hepatic fat is concerning, the immediate focus should be on more dominant risk factors like visceral fat. They suggest a tiered approach to screening, prioritizing resources for the most severe threats while gradually building awareness about liver health. This pragmatic stance reflects the realities of strained medical systems but risks delaying action on a growing problem.
Moving Beyond BMI: Rethinking Obesity Metrics
The inadequacy of BMI as a standalone measure of heart risk is a point of near-universal agreement among health experts. Recent analyses show that surface-level metrics like waist circumference often fail to account for internal fat deposits that drive artery damage. Specialists in diagnostic technology are pushing for advanced imaging methods, such as MRI scans, to become a standard part of cardiovascular risk assessment, even for those who appear fit.
Global health researchers add that this shift away from BMI aligns with emerging trends in metabolic health, where fat distribution matters more than total body weight. They predict that within the next few years, from 2025 to 2027, imaging could redefine how obesity is evaluated across different regions, potentially reducing misdiagnoses. Their optimism is tempered by concerns over cost and accessibility, which remain barriers to widespread adoption.
A dissenting opinion comes from some traditional clinicians who caution against over-reliance on high-tech solutions. They argue that while BMI has flaws, it still serves as a useful starting point for identifying at-risk patients when combined with other basic tests. This perspective calls for a balanced approach, integrating new tools without discarding established methods entirely, to ensure broader reach in diverse healthcare settings.
Hidden Fat Across Populations: A Shared Concern
The impact of hidden fat on artery health transcends geographic and genetic boundaries, a finding echoed by epidemiologists studying varied lifestyles. Large-scale data indicate consistent associations between visceral fat and cardiovascular damage, whether in urban or rural settings, among different ethnic groups. Public health officials note that this universality demands a global response, prioritizing awareness campaigns that cut across cultural norms.
Some behavioral scientists, however, point out that society’s obsession with external appearance often overshadows internal health risks. They advocate for a cultural shift to focus on metabolic wellness rather than weight loss alone, suggesting tailored messaging to combat stigma around body image. Their view adds a psychological dimension to the discussion, urging a rethink of how health priorities are communicated.
Contrarily, a few policy analysts warn that universal approaches may overlook local disparities in healthcare access and education. They propose region-specific strategies to address hidden fat risks, ensuring that solutions account for economic and systemic differences. This nuanced take emphasizes customization over a one-size-fits-all model, sparking debate on how best to implement change on a worldwide scale.
Practical Takeaways for Addressing Hidden Fat Risks
Health professionals across disciplines agree on the urgent need to confront the dangers of visceral and hepatic fat through updated practices. Cardiologists recommend that healthcare providers adopt imaging-based diagnostics to detect internal fat deposits, especially for patients with no visible weight gain but other subtle risk factors. This shift could redefine routine screenings, catching threats before they escalate into serious conditions.
For individuals, nutrition and fitness experts suggest proactive steps like discussing hidden fat with doctors during annual checkups, even if body weight seems normal. They also advise focusing on diets low in processed foods and high in fiber to reduce fat accumulation over time. These practical tips empower people to take charge of their metabolic health beyond superficial measures.
A complementary perspective from preventive medicine specialists highlights the importance of community-level interventions. They call for public health programs to educate about the risks of internal fat, integrating such knowledge into school curricula and workplace wellness initiatives. This broader approach aims to build a foundation of awareness that supports both clinical and personal efforts to mitigate cardiovascular risks.
Reflecting on the Collective Wisdom of Hidden Fat Research
Looking back, the diverse insights gathered from researchers, clinicians, and health advocates paint a comprehensive picture of the silent threat posed by hidden fat to artery health. Discussions ranged from the undeniable dangers of visceral and hepatic fat to the shortcomings of BMI, revealing a shared urgency to overhaul how cardiovascular risks are assessed. The varied opinions underscored a complex challenge that demands both innovation and practicality in equal measure.
Moving forward, the next steps lie in bridging the gap between cutting-edge diagnostics and everyday healthcare access, ensuring that advanced imaging becomes a feasible option for more people. Exploring further readings on metabolic health and advocating for policy changes to fund such technologies can sustain the momentum of this critical conversation. Addressing hidden fat remains an evolving journey, one that calls for continued collaboration across medical and societal spheres to protect heart health on a global scale.