For individuals living with debilitating genetic skin disorders, effective treatments have remained elusive, often limited to managing symptoms rather than addressing the root cause encoded in their DNA. A groundbreaking development from researchers at the University of British Columbia and the Berlin Institute of Health at Charité, however, heralds a new era in dermatology. They have successfully engineered the first-ever topical gene therapy that employs CRISPR technology to correct disease-causing mutations directly within the skin. This pioneering work, detailed in a study published in Cell Stem Cell, bypasses the systemic risks associated with traditional gene therapies by delivering the corrective machinery precisely where it is needed. The innovation not only offers a potential permanent cure for a range of inherited skin conditions but also establishes a novel platform for treating genetic diseases in a localized, non-invasive manner, promising to transform the lives of patients who have long been without hope for a definitive solution.
A Novel Delivery System
Overcoming the Skin’s Barrier
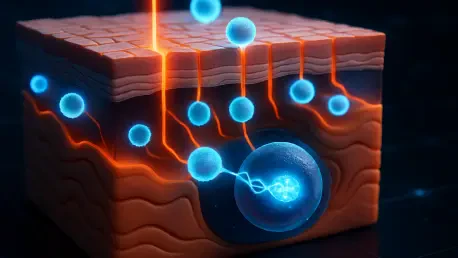
The primary obstacle in developing effective topical gene therapies has always been the skin’s formidable natural defenses, particularly the outermost layer known as the stratum corneum, which is expertly designed to keep foreign substances out. To circumvent this biological fortress, the research team devised an elegant and sophisticated two-step delivery method that ensures the therapeutic agents reach their intended targets deep within the skin’s layers. The initial step involves the use of a clinically approved laser to create microscopic, pain-free openings in the epidermis. This technique, known as fractional laser ablation, is already used in cosmetic dermatology and is well-tolerated by patients. The micro-perforations are incredibly small and heal quickly, but they serve as crucial conduits, temporarily opening a direct pathway for the subsequent therapeutic formulation to penetrate beyond the surface and access the underlying basal layer where skin stem cells reside. This precise and minimally invasive preparation of the skin is the critical first stage that enables the entire gene-editing process to succeed.
The second, and equally crucial, component of the system is the topical formulation itself, which contains the powerful CRISPR gene-editing tools. To protect and transport this delicate molecular machinery, the scientists utilized lipid nanoparticle (LNP) technology, the same innovative “bubbles of fat” that proved instrumental in the global success of mRNA vaccines. These LNPs encapsulate the gene-editing components, shielding them from degradation and facilitating their passage into the cells. Once the LNP-laden cream is applied to the laser-treated area, the nanoparticles travel through the microscopic channels and are absorbed by the skin stem cells. Inside these cells, the LNPs release their cargo, and the CRISPR machinery gets to work. It acts like a pair of molecular scissors, precisely finding the faulty segment of DNA responsible for the genetic disorder, cutting it out, and allowing the cell’s natural repair mechanisms to fix the gene using a correct template. This targeted approach ensures that the genetic correction occurs specifically in the long-lived stem cells that are responsible for regenerating the skin.
Proving Efficacy in a Rare Disease
To validate their innovative therapeutic approach, the researchers focused on autosomal recessive congenital ichthyosis (ARCI), a severe and rare inherited skin disorder for which no cure currently exists. Affecting approximately one in every 100,000 individuals, ARCI manifests as extremely dry, thick, and scaly skin that resembles fish scales. This condition results from genetic mutations that disrupt the normal shedding process of skin cells, leading to a dysfunctional skin barrier. Patients with ARCI suffer from chronic inflammation, a persistent risk of life-threatening infections, and significant physical discomfort and social stigma. By selecting ARCI as their initial target, the team aimed to demonstrate the therapy’s potential to address a condition with a clear genetic origin and a high unmet medical need. The study specifically targeted the most common genetic mutation responsible for the disease, providing a clear and measurable endpoint to assess the efficacy of the topical CRISPR treatment in a clinically relevant context.
The experimental results provided compelling evidence of the therapy’s success. Using models constructed from living human skin tissues derived from ARCI patients, the team applied the two-step treatment process. Following the application, analysis revealed that the CRISPR-LNP formulation had successfully corrected the target genetic mutation. More importantly, this genetic correction translated into a functional restoration of the skin. The treated skin models showed a significant improvement in barrier function, with the therapy restoring up to 30 percent of normal activity. According to previous dermatological research, achieving this level of functional restoration is considered clinically meaningful and is believed to be sufficient to return the skin to a healthy, functional state. This outcome represents a monumental step forward, demonstrating for the first time that a topical, non-invasive gene-editing treatment can reverse the molecular and functional deficits of a debilitating genetic skin disease directly in human tissue.
The Broader Implications and Future Path
Safety and Long-Term Potential
A paramount concern for any therapy involving gene editing is safety, particularly the risk of “off-target” effects where the CRISPR system might unintentionally alter other parts of the genome. The study meticulously investigated this possibility and yielded highly encouraging results. The researchers found no evidence of off-target mutations in the treated skin models, a critical safety milestone that underscores the precision of their system. Furthermore, because the therapy is applied topically, its effects are highly localized to the treated area of the skin. This containment significantly reduces the risk of systemic exposure and unintended consequences in other organs or tissues, a major advantage over gene therapies that are delivered intravenously and circulate throughout the body. This combination of high precision and localized action provides a strong safety profile, which will be essential as the therapy moves toward clinical trials and potential use in human patients. The ability to safely edit genes in a specific tissue without systemic risk is a long-sought goal in the field.
Beyond its immediate efficacy and safety, the most promising aspect of this new therapy is its potential for providing a lasting, durable cure. The treatment is specifically designed to target the long-living stem cells located in the basal layer of the epidermis. These cells are the regenerative engines of the skin, continuously producing new cells to replenish the outer layers. By correcting the genetic mutation at its source within this foundational cell population, the therapeutic effect becomes self-renewing. As these corrected stem cells divide and differentiate, they give rise to healthy, genetically normal skin cells that will eventually replace the entire epidermis in the treated area. Consequently, the researchers suggest that a single application of the therapy could be sufficient to provide a permanent solution. This “one-and-done” treatment paradigm stands in stark contrast to existing palliative treatments for genetic skin disorders, which require lifelong, continuous application to merely manage symptoms without ever addressing the underlying genetic defect.
A Platform for Widespread Application
The creators of this therapy emphasize that its true power lies in its versatility as a “platform technology.” While the initial study focused on ARCI, the fundamental delivery system—combining a laser-assisted approach with a CRISPR-LNP formulation—is not limited to a single disease or gene. The system is readily adaptable to treat a vast array of other genetic skin conditions. The core principle involves simply reprogramming the CRISPR tool’s guide RNA to recognize and target a different faulty gene. This modular design means that developing a new treatment for another genetic skin disorder would not require reinventing the entire delivery mechanism, but rather substituting a new set of genetic instructions. This adaptability dramatically accelerates the potential timeline for creating new therapies for conditions like epidermolysis bullosa, a brutal disorder known as ‘butterfly skin’ where the skin is extraordinarily fragile, as well as other rare inherited diseases that currently have no effective treatments.
The successful demonstration of this technology marked a pivotal moment, shifting the project from preclinical research toward clinical reality. In a collaborative effort with NanoVation Therapeutics, a UBC spin-off company dedicated to advancing this delivery platform, the research team has begun the crucial process of translating their laboratory findings into a treatment for patients. This next phase involved initiating discussions with regulatory authorities to meticulously plan the necessary safety and efficacy studies required for first-in-human clinical trials. The development of this adaptable and localized gene-editing system established a clear and promising path forward, offering a tangible strategy to address a wide spectrum of both rare and common skin disorders, including complex conditions like eczema and psoriasis which have genetic components. This research laid the essential groundwork for transforming the treatment landscape for patients who have long awaited a breakthrough.