What if a diagnostic tool could save lives by detecting prostate cancer just as effectively, but in half the time and at a fraction of the cost? This isn’t a distant dream but a reality unveiled through a groundbreaking clinical trial that’s turning heads in the medical community. Prostate cancer, a leading health concern for men globally, often goes undetected due to barriers like high costs and long wait times for scans. A new MRI technique promises to shatter these obstacles, offering hope to millions who need timely diagnosis.
Why This Matters: The Prostate Cancer Crisis
Prostate cancer stands as the most common cancer among men in the UK, with around 56,000 new cases and 12,000 deaths reported each year. The disease’s silent progression means early detection is critical, yet many men face significant hurdles in accessing necessary screenings. MRI scans have become a cornerstone of diagnosis, guiding doctors to suspicious areas for biopsy, but the system is strained by limited resources and escalating demand.
The gap in access is stark. Current data reveals that a significant percentage of men who need an MRI don’t receive one, with systemic issues like staffing shortages and expensive procedures creating bottlenecks. This disparity leaves countless individuals at risk of delayed diagnosis, amplifying the urgency for a solution that can scale to meet global needs without sacrificing accuracy.
Breaking New Ground: The PRIME Trial Unveiled
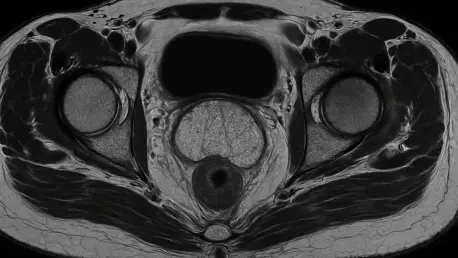
Enter the PRIME trial, a pioneering study led by researchers from University College London and the University of Birmingham, spanning 22 hospitals across 12 countries. This international effort tested a novel approach called biparametric MRI, a streamlined two-part scan, against the traditional three-part multiparametric MRI. With 555 participants aged 59-70, the trial delivered a stunning result: both methods detected significant prostate cancer in 29% of patients, proving their equal effectiveness.
What sets this new technique apart is its efficiency. The biparametric MRI cuts scan times from 30-40 minutes down to 15-20 minutes and slashes costs by 47% within the UK’s National Health Service, reducing per-scan expenses from £273 to £145. By eliminating the contrast dye injection stage, it also reduces the need for specialized staff, addressing a key barrier in under-resourced healthcare settings.
The implications are profound. This innovation not only maintains diagnostic precision but also opens doors for broader implementation, potentially transforming how hospitals manage their imaging workloads. It’s a step toward ensuring that more men can access life-saving screenings without the burden of prohibitive costs or endless delays.
Voices from the Frontlines: Experts Weigh In
Associate Professor Veeru Kasivisvanathan, a lead investigator in the PRIME trial, underscores the transformative potential of this advancement: “This quicker, more affordable scan meets the rising demand for prostate cancer diagnostics while upholding the highest standards of accuracy.” His perspective highlights a critical shift in how healthcare systems could adapt to growing challenges with smarter solutions.
Lead radiologist Associate Professor Francesco Giganti adds a layer of nuance, stressing that image quality remains paramount. “Even with a simplified protocol, expert interpretation and optimal scanning techniques are non-negotiable,” he notes. This insight serves as a reminder that technology must be paired with skilled professionals to achieve the best outcomes.
Advocacy groups are equally vocal about the need for rapid change. Dr. Matthew Hobbs from Prostate Cancer UK urges immediate action, calling on the National Institute for Health and Care Excellence to update clinical guidelines. His push reflects a broader sentiment that research must translate into real-world impact swiftly, especially for men in regions where access to standard MRI scans remains a distant possibility.
Real-World Impact: Changing Lives and Systems
For hospitals, the biparametric MRI offers a tangible opportunity to revolutionize patient care. By adopting this method, facilities can double the number of daily scans, addressing backlogs that leave patients waiting for weeks or even months. Training radiologists to maintain high-quality imaging without contrast dye, as supported by complementary studies like the GLIMPSE trial, is a practical first step that administrators can prioritize now.
Patients, too, stand to gain immensely. The reduced cost and shorter scan duration mean less financial strain and quicker answers during a time of uncertainty. Men concerned about prostate health are encouraged to discuss with their healthcare providers whether this innovative scan is available at their local facilities, advocating for access to cutting-edge diagnostics.
Beyond individual benefits, the international scope of the PRIME trial signals its relevance to diverse healthcare systems. In areas with limited resources, where even basic MRI machines are scarce, this streamlined approach could be a game-changer, ensuring that life-saving technology reaches those who need it most, regardless of geography or economic status.
A Path Forward: Building on the Breakthrough
Looking back, the PRIME trial marked a turning point in prostate cancer diagnostics, demonstrating that efficiency and accuracy could coexist in a field often constrained by resource limitations. The evidence was clear: a faster, cheaper MRI scan held its ground against the traditional standard, paving the way for systemic improvements. Hospitals and advocacy groups rallied behind the findings, eager to see them integrated into everyday practice.
The next steps demanded action on multiple fronts. Healthcare providers were tasked with updating protocols and training staff to implement the biparametric MRI effectively, while policymakers faced pressure to revise guidelines for broader adoption. For patients, staying informed and proactive became crucial—asking questions and seeking out facilities offering this advanced scan could make all the difference.
As ongoing research, such as the TRANSFORM trial, continued to explore national screening strategies, the momentum built by this breakthrough offered a glimpse of a future where no man would be left behind due to cost or wait times. The journey toward equitable, accessible prostate cancer care took a significant leap forward, with the promise of saving more lives through innovation and collaboration.