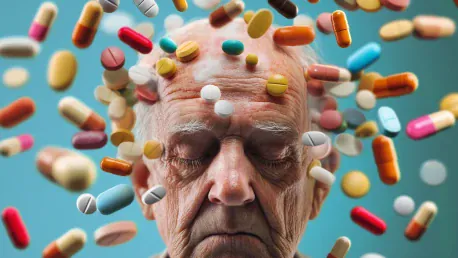
The ethical concerns surrounding the non-disclosure of genetic risks to participants in Alzheimer’s anti-amyloid drug trials have sparked significant debate. Eisai and Eli Lilly, the companies conducting these trials, were aware of the increased risk of brain swelling and bleeding in participants who had two copies of the APOE4 gene. However, despite knowing this, they chose not to inform the participants during the trial period. This decision has led to questions about the ethical standards in place and the necessity of informed consent.
The Importance of Informed Consent
Definition and Significance of Informed Consent
Informed consent is a crucial element in clinical trials, ensuring that participants are made fully aware of all potential risks, uncertainties, and benefits associated with a treatment. This process allows participants to make an educated decision on whether or not to take part in a trial. In the case of the Alzheimer’s drug trials, about one in six volunteers were APOE4 homozygotes who were not informed about their increased risk of side effects. The non-disclosure of such critical information raises serious ethical questions about the integrity of the informed consent process. Ensuring that participants have access to all relevant information is fundamental to respecting their autonomy and safeguarding their well-being.
Informed consent is not just a formal requirement; it’s a cornerstone of ethical medical practice. When participants agree to take part in clinical trials, they entrust researchers with significant responsibility over their health and personal information. In the Alzheimer’s drug trials by Eisai and Eli Lilly, the omission of genetic risk information threatened this trust. The companies neglected to provide volunteers with the necessary knowledge to make informed decisions about their participation. Such an omission can undermine confidence in medical research and highlight the need for stringent ethical standards to protect participants.
Ethical Standards and Non-Disclosure
Ethical standards for clinical trials dictate the obligation of researchers to disclose known risks to participants. Some experts argue that by withholding this critical piece of information, participants’ consent was not truly “informed.” They maintain that the undisclosed genetic information undermined participant autonomy and violated the ethics of informed consent. These ethical principles are intended to ensure transparency and protect the rights of participants, enabling them to assess the potential risks and benefits accurately.
Failing to disclose important genetic risks not only breaches these ethical standards but also jeopardizes the trust placed by participants in the research process. The non-disclosure by Eisai and Eli Lilly raises important questions about the ethical frameworks governing clinical trials. It highlights the need for strict adherence to ethical guidelines that prioritize participant safety and informed decision-making. Ethical lapses in such scenarios can result in unintended harm and diminish the credibility of clinical research, underscoring the importance of robust ethical oversight.
Expert Opinions on Non-Disclosure
Criticism from Ethical Experts
Several experts strongly condemn the non-disclosure practice, highlighting its ethical flaws and the deception it represented to the participants. Dr. George Perry described the act as “ethically fraught,” emphasizing the significance of patient autonomy and informed consent. Carl Elliot noted that deceiving participants and withholding critical health information was disgraceful and wrong, attributing such decisions to deeper systemic issues in the clinical research ethics approval system. These critical viewpoints underscore the ongoing debate about the ethical responsibilities of researchers and the potential consequences of neglecting informed consent.
The sharp criticism from ethical experts reflects broader concerns about the impact of non-disclosure on the integrity of clinical research. Dr. Perry and Carl Elliot argue that failing to inform participants about their genetic risks compromises their ability to make autonomous decisions about their health. This disregard for patient autonomy is seen as a significant ethical violation that undermines the foundational principles of medical research. Such concerns highlight the need for greater scrutiny and reform to prevent similar ethical breaches in future clinical trials.
Defense of Non-Disclosure
Opposing views suggest that, when these trials were initiated, the link between APOE4 and ARIA wasn’t as clearly established as it is now. Dr. Scott Roberts from the University of Michigan and Dr. David Weisman from Abington Neurological Associates argue that the understanding of genetic risks was still evolving during these trials, thus, the non-disclosure could have been deemed scientifically and ethically acceptable at that time. They point out that the trials themselves contributed to the growing body of knowledge relating to the genetic risks, which has since become more clearly defined.
This perspective suggests that the non-disclosure was not a deliberate attempt to deceive participants but a reflection of the evolving scientific understanding at the time. Dr. Roberts and Dr. Weisman emphasize that the landscape of genetic research is constantly changing, and ethical standards must adapt accordingly. Their defense highlights the complexities inherent in conducting clinical trials, where researchers must often balance emerging scientific insights with established ethical guidelines. This nuanced view underscores the ongoing need for dynamic ethical frameworks that respond to advancements in medical research.
The Evolution of Genetic Risk Disclosure
The REVEAL Study and Its Findings
Dr. Robert C. Green’s REVEAL study initially sought to understand the psychological impact of disclosing genetic risk factors like APOE4. The study found that disclosing such risks did not result in significant psychological distress among patients, contrary to earlier beliefs. Green posits that the notion of non-disclosure is a leftover from earlier days when it was feared that disclosing genetic information would cause severe psychological harm. These findings challenge previous assumptions and advocate for greater transparency in communicating genetic risks.
The REVEAL study’s findings have significant implications for the ethical standards of clinical trials. Dr. Green’s work demonstrates that participants can handle the psychological impact of learning about their genetic risks and that withholding such information may no longer be justified. This shift in understanding supports the need for updated ethical frameworks that prioritize transparency and respect for participant autonomy. The insights gained from the REVEAL study help inform the ongoing debate about genetic risk disclosure and its importance in clinical research.
Shift Towards Transparency
Despite conflicting viewpoints, the overarching trend in the field has shifted towards transparency in recent years. Currently, it is standard practice to disclose APOE4 status to participants prior to the commencement of anti-amyloid clinical trials. Drug companies now seek informed consent by offering prospective participants the option to learn their genetic profiles beforehand. This shift demonstrates a growing emphasis on ethical considerations and the importance of providing participants with comprehensive information about their genetic risks.
The move towards greater transparency reflects a broader trend in medical research that prioritizes patient autonomy and informed decision-making. By disclosing genetic risks upfront, researchers aim to foster trust and encourage more informed participation in clinical trials. This practice ensures that participants can make well-informed decisions about their involvement, balancing the potential benefits of the trial with the known risks. The emphasis on transparency signifies an important evolution in the ethical standards governing clinical research, highlighting the need for continued ethical vigilance.
Institutional Review Boards and Ethical Oversight
Concerns Over For-Profit Review Boards
The U.S. Government Accountability Office raised concerns about for-profit institutional review boards, such as Advarra, which approved the ethical considerations of these trials. This raises additional ethical concerns regarding the oversight and motivations when private firms are involved in the ethics approval processes. The involvement of for-profit entities in ethical review can introduce potential conflicts of interest, which may compromise the integrity of the review process and undermine participant protection.
Ethical oversight is a critical component of ensuring that clinical trials adhere to high standards of transparency and participant safety. The concerns raised about for-profit review boards highlight the potential risks associated with entrusting ethical review to entities with financial interests. These concerns underscore the need for stringent oversight and regulatory frameworks to ensure that ethical considerations are not compromised by profit motives. Addressing these issues is vital for maintaining public trust in the clinical research process and protecting participant rights.
The Role of Review Boards in Ensuring Ethical Standards
Review boards play a critical role in ensuring that clinical trials adhere to ethical standards. The involvement of for-profit entities in this process can lead to potential conflicts of interest, which may compromise the integrity of the ethical review process. This highlights the need for stringent oversight and transparency in the approval of clinical trials. Ensuring robust ethical oversight is essential for safeguarding participant welfare and maintaining the credibility of clinical research.
Stringent regulatory frameworks and the inclusion of independent review boards are necessary to mitigate potential conflicts of interest in the ethical review process. Transparent and unbiased reviews are crucial for protecting participant rights and upholding ethical standards. The involvement of for-profit entities must be carefully monitored to prevent any compromise of the ethical integrity of clinical trials. Ensuring impartial and thorough ethical reviews can help address the concerns raised and reinforce the commitment to ethical research practices.
Current Practices and Future Directions
Emphasis on Patient Autonomy
The growing consensus now leans towards full transparency and proactive communication regarding genetic risks, ensuring informed consent that respects and empowers trial participants. Experts like Dr. Jason Karlawish advocate for providing potential trial participants with all the necessary information to make an informed decision about their participation, underscoring the importance of balancing potential benefits with known risks. This approach emphasizes the need for ethical practices that prioritize participant autonomy and informed decision-making in clinical trials.
By placing a strong emphasis on patient autonomy, the field of clinical research aims to build trust and encourage more informed participation. Providing comprehensive information about genetic risks allows participants to weigh the potential benefits and make choices that align with their values and preferences. Dr. Karlawish’s advocacy for transparent and ethical practices reflects the evolving standards in clinical research, highlighting the importance of respecting participant rights and promoting informed consent.
Responses from Eisai and Eli Lilly
The issue of not disclosing genetic risks to participants in Alzheimer’s anti-amyloid drug trials has ignited notable ethical discussions. Eisai and Eli Lilly, the pharmaceutical companies running these trials, were aware that participants with two copies of the APOE4 gene had a higher risk of brain swelling and bleeding. Nevertheless, they opted not to inform the participants of these risks during the trial phase. This decision has raised serious questions about ethical practices within clinical trials and the essential role of informed consent. The potential consequences of withholding such critical information have prompted a broader conversation about the responsibilities of drug companies to ensure that participants are fully aware of all risks involved. This situation underscores the ongoing debate in the medical community about how best to balance scientific progress with patient safety and rights, emphasizing the need for stringent ethical standards and transparency in clinical research.