In the realm of regenerative medicine, a staggering challenge persists: millions of patients worldwide suffer from vascular diseases, awaiting solutions that can repair or replace damaged blood vessels, while endothelial cells, which form the critical inner lining of these vessels, hold the key to transformative treatments. Yet, their cultivation in sufficient quantities for clinical use has long eluded scientists. This review delves into a pioneering technology developed at Weill Cornell Medicine that achieves large-scale production of these vital cells, offering hope for personalized therapies in vascular health, organ transplantation, and cancer treatment. The focus here is to unpack this innovation, assess its capabilities, and evaluate its potential to redefine medical practice.
Understanding the Core of Endothelial Cell Technology
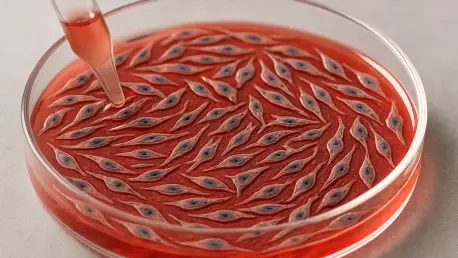
Endothelial cells serve as the gatekeepers of blood vessels, regulating blood flow, managing inflammation, and aiding in tissue repair. Historically, growing these cells in a lab setting for therapeutic purposes has been fraught with obstacles, as they often lose functionality or become unstable after limited divisions. The breakthrough at hand introduces a method to propagate human endothelial cells on an unprecedented scale, starting from just a small biopsy sample, while preserving their integrity and purpose.
This technology tackles a decades-long barrier by enabling the production of vast quantities of patient-specific cells. Unlike previous approaches where cells from sources like umbilical cords quickly reached senescence, this method awakens dormant adult cells, making it feasible to apply in real-world clinical scenarios. The significance lies not only in the volume but also in maintaining the cells’ ability to form functional blood vessels, a critical factor for safe medical applications.
Key Features and Mechanisms of the Innovation
Targeting the Aryl Hydrocarbon Receptor Pathway
At the heart of this advancement is the use of small molecule inhibitors that target the aryl hydrocarbon (AH) receptor pathway, a signaling mechanism previously linked to gene regulation. By inhibiting this pathway, the technology prompts dormant endothelial cells to multiply extensively, achieving up to 2 trillion cells from a single sample—a hundredfold increase over traditional methods. Remarkably, the cells show no signs of aging or genetic instability during this massive expansion.
The importance of this feature cannot be overstated. Maintaining genomic stability ensures that the cells remain safe for therapeutic use, avoiding risks of mutations that could lead to adverse outcomes. This precise targeting represents a leap forward, transforming a once theoretical possibility into a tangible tool for regenerative medicine.
Uncovering a Non-Canonical Mechanism
Beyond the initial discovery, an unexpected aspect emerged: the inhibitors do not simply block the AH receptor’s typical activity but activate an alternative pathway. This non-canonical mechanism alters cellular metabolism, reduces harmful oxidative stress, and boosts polyamine production, a compound essential for cell growth. Such findings challenge prior scientific assumptions about how these pathways operate.
This deeper understanding of cellular behavior opens new avenues for research. It highlights the complexity of biological systems and underscores the value of exploratory science in uncovering hidden mechanisms. The ability to reduce oxidative damage while sustaining cell proliferation adds a layer of robustness to the technology, enhancing its reliability for clinical translation.
Performance in Scalability and Clinical Potential
The standout performance metric of this cultivation method is its scalability, producing quantities of endothelial cells previously unimaginable for patient-specific therapies. This capability directly addresses the growing demand for tailored treatments in vascular conditions like heart disease, where vascular grafts could restore blood flow. Additionally, it holds promise for diabetes management by supporting tissue repair and improving blood supply to affected areas.
In broader applications, the technology shows potential in organ transplantation by enabling the creation of blood vessel networks to support transplanted tissues. Another compelling use case lies in cancer therapy, where targeting tumor vasculature with engineered cells could disrupt the blood supply fueling malignant growth. These diverse possibilities illustrate the versatility of the method across multiple medical domains.
However, performance is not without challenges. Ensuring consistent clinical-grade quality during such large-scale expansion remains a technical hurdle. Variations in cell behavior or unintended off-target effects of the inhibitors require rigorous monitoring to meet regulatory standards. Ongoing refinements aim to address these issues, striving for seamless integration into medical practice.
Limitations and Areas for Improvement
Despite its groundbreaking nature, the technology faces limitations in maintaining absolute uniformity across expanded cell populations. Minor inconsistencies in cell stability during massive propagation can pose risks if not carefully controlled, potentially affecting therapeutic outcomes. This necessitates advanced quality assurance protocols to detect and mitigate any deviations early in the process.
Regulatory barriers also loom large, as achieving approval for widespread clinical use involves demonstrating long-term safety and efficacy across diverse patient groups. The complexity of scaling production while adhering to stringent guidelines adds another layer of difficulty. Efforts are underway to streamline these processes, ensuring that the innovation can transition from lab to bedside efficiently.
Cost considerations further complicate adoption. Developing infrastructure for large-scale cultivation and inhibitor production may require significant investment, potentially limiting access in resource-constrained settings. Addressing affordability through optimized manufacturing and strategic partnerships will be crucial to democratizing this life-changing technology.
Future Directions and Emerging Trends
Looking ahead, the trajectory of this technology points toward deeper exploration of the AH receptor pathways to uncover additional mechanisms that could enhance efficiency. Research over the coming years, from 2025 onward, will likely focus on tailoring cultivation for tissue-specific applications, such as engineering blood vessels suited for particular organs. This customization could revolutionize replacement therapies with durable, functional outcomes.
Another trend shaping the field is the integration of this method with other regenerative approaches, such as 3D bioprinting, to construct complex vascular structures. Combining these innovations could accelerate the development of fully functional artificial organs. The emphasis on patient-specific solutions aligns with broader shifts in healthcare toward personalized medicine, positioning this technology at the forefront of medical evolution.
Collaboration across disciplines will play a vital role in overcoming existing barriers. Partnerships between researchers, clinicians, and regulatory bodies can facilitate faster validation and implementation, ensuring that the benefits reach patients sooner. Keeping pace with these trends will be essential to maximize the impact of endothelial cell cultivation on global health.
Final Thoughts on a Transformative Technology
Reflecting on this remarkable advancement, the technology for large-scale endothelial cell cultivation stands as a game-changer in regenerative medicine. Its ability to produce vast quantities of functional cells from minimal starting material marks a turning point in addressing vascular and organ-related challenges. The unexpected discovery of alternative pathways enriches scientific knowledge, while its clinical applications promise to reshape treatment landscapes.
Moving forward, the next steps involve intensifying research to refine inhibitor mechanisms and ensure scalability without compromising quality. Establishing robust frameworks for regulatory approval and cost reduction emerges as critical priorities to broaden access. Ultimately, fostering global collaboration to integrate this innovation into routine care offers the clearest path to transforming patient outcomes in vascular health and beyond.