Sophisticated nanodelivery systems that respond to multiple biological cues are rapidly redefining the landscape of targeted therapeutics, offering a highly precise method for overcoming the formidable barriers presented by diseases like metastatic cancer. This review explores the evolution of these dual-responsive platforms, detailing their fundamental design principles, performance metrics, and transformative impact on applications ranging from oncology to immunotherapy. The purpose is to provide a comprehensive analysis of the technology’s current capacity to navigate biological complexities and its potential for future clinical translation, ultimately aiming to enhance treatment efficacy and patient outcomes.
Fundamentals of Dual-Responsive Nanodelivery
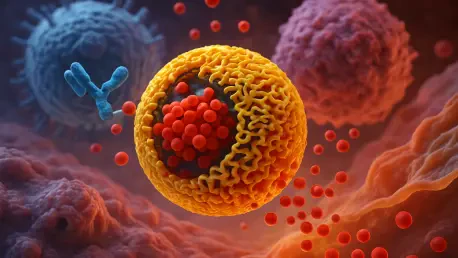
Dual-responsive nanodelivery technology represents a pivotal shift from conventional drug administration and single-stimulus systems by incorporating sensitivity to two distinct triggers. Its core principle lies in creating a nanocarrier that remains stable and inert in healthy physiological conditions but undergoes specific structural changes when it encounters a unique combination of signals characteristic of a disease site, such as a tumor microenvironment. This multi-layered activation mechanism addresses the limitations of less sophisticated systems, which often suffer from premature drug leakage or insufficient payload release at the target.
By requiring two separate environmental cues for activation, these systems achieve an unparalleled level of precision and control. For instance, one stimulus might trigger accumulation at the target tissue, while a second, intracellular stimulus prompts the release of the therapeutic payload directly inside the diseased cells. This sequential action not only maximizes the drug concentration where it is needed most but also minimizes off-target effects and systemic toxicity, a critical challenge in potent treatments like chemotherapy and immunotherapy. This approach transforms the nanocarrier from a passive delivery vehicle into an intelligent, active participant in the therapeutic process.
Design Principles and Mechanistic Action
Integrating Endogenous and Exogenous Triggers
The power of dual-responsive systems originates from the strategic integration of triggers, which can be categorized as either endogenous (internal to the body) or exogenous (applied externally). Endogenous stimuli are naturally occurring signals within specific biological niches, such as the acidic pH, high glutathione (GSH) concentrations, or elevated enzyme levels found within the tumor microenvironment (TME). In contrast, exogenous stimuli like light, temperature, or ultrasound offer external, on-demand control over drug release.
The combination of two distinct triggers enables a highly specific and sequential release of therapeutic agents. For example, a nanocarrier might be designed to first leverage the acidic pH of the TME to shed a protective outer layer and facilitate cellular uptake. Once inside the cell, it could then respond to the high intracellular GSH concentration, triggering the cleavage of disulfide bonds to release its payload. This lock-and-key approach ensures that the therapeutic action is confined precisely to the target cells, overcoming the biological complexity that often renders single-stimulus systems ineffective.
Crafting the Nanocarrier and Co-Loading Therapeutics
The nanocarrier itself is a feat of molecular engineering, constructed from carefully selected components to achieve the desired responsiveness and stability. Polymers like polycaprolactone (PCL) and polyethylene glycol (PEG) form the structural backbone, while targeting ligands such as mannose are incorporated to guide the nanoparticle to specific receptors on cancer cells. The self-assembly of these components results in a nanoparticle with precisely controlled physicochemical properties, including size, surface charge, and drug-loading capacity. For instance, a system can be designed to have a negative charge in the bloodstream to avoid non-specific interactions but reverse to a positive charge in the acidic TME to enhance cellular internalization.
A key advantage of these platforms is their ability to co-load multiple therapeutic agents with different mechanisms of action, enabling synergistic combination therapies. This is exemplified by systems carrying STING agonists like diABZI to activate innate immunity, ferroptosis inducers like IKE to promote a specific type of cancer cell death, and immune checkpoint inhibitors like aPD-1 to release the brakes on the adaptive immune response. The final formulation, such as the MPP@IKE-aPD-1/diABZI system, exhibits a well-defined spherical morphology under 100 nm, ensuring optimal circulation and tumor penetration, while its engineered structure prevents premature drug leakage and guarantees release only upon encountering the dual pH and GSH triggers.
Emerging Trends in Multifunctional Nanosystems
The latest developments in dual-responsive technology are pushing the boundaries of what a nanosystem can achieve, moving beyond simple drug delivery toward truly multifunctional platforms. A major trend is the integration of disparate therapeutic modalities to create synergistic effects that a simple drug cocktail could not produce. This includes combining ferroptosis-inducing agents with immunotherapy to not only kill tumor cells directly but also trigger an immunogenic cell death that primes the immune system for a more robust anti-tumor response.
Furthermore, next-generation systems are being designed to actively regulate and remodel the immune microenvironment. Instead of just delivering a payload, these nanoplatforms can be engineered to reprogram immunosuppressive cells, enhance the infiltration of cytotoxic T-cells, and promote the maturation of dendritic cells. This active participation turns the tumor from a “cold,” immune-excluded environment into a “hot,” immune-inflamed one, making it far more susceptible to immunotherapies. Such innovations mark a transition from passive delivery vehicles to dynamic therapeutic agents.
In Vivo Performance and Therapeutic Applications
Enhancing Anti-Tumor Efficacy in Oncology
The real-world potential of dual-responsive nanodelivery is strikingly illustrated in preclinical models of aggressive cancers, such as metastatic bladder cancer. In these studies, combination formulations have demonstrated robust and superior tumor control, achieving inhibition rates exceeding 90%. This remarkable efficacy stems from the system’s ability to deliver a multi-pronged attack directly to the tumor site, overwhelming cancer cells’ defense mechanisms and simultaneously activating a powerful anti-tumor immune response.
This enhanced efficacy translates directly into significant survival benefits. Animal models treated with these advanced nanosystems show substantially prolonged median survival compared to control groups or those receiving single-agent therapies. The underlying mechanism involves a profound remodeling of the TME, characterized by a dramatic increase in mature, antigen-presenting dendritic cells and a massive influx of tumor-killing CD8+ T-cells. This coordinated biological response underscores the power of delivering synergistic agents to the right place at the right time.
Overcoming Metastasis and Establishing Immune Memory
Beyond treating the primary tumor, a critical application for these nanosystems is in combating metastasis, the primary cause of cancer-related mortality. By targeting both the primary tumor and lymph nodes, these platforms can effectively shut down the pathways of cancer spread. In spontaneous metastasis models, treatment has led to a drastic reduction in the number of metastatic nodules in distant organs like the lungs, showcasing the technology’s potential to manage advanced, disseminated disease.
Perhaps most importantly, these systems have proven capable of establishing durable, long-term immune memory. After the initial tumor is cleared, the immune system remains vigilant, with elevated levels of central and effector memory T-cells circulating throughout the body. In rechallenge experiments, where animals are re-exposed to tumor cells long after the initial treatment, this immune memory prevents new tumors from forming. This induction of a vaccine-like effect represents a crucial step toward achieving lasting cures and preventing disease recurrence.
Current Challenges and Translational Hurdles
Biocompatibility and Systemic Toxicity Concerns
Despite their promise, dual-responsive nanosystems face significant technical and biological challenges on the path to clinical use. A primary concern is their long-term biocompatibility and potential for systemic toxicity. While designed for targeted release, unintended systemic exposure can still occur, and the accumulation of nanoparticle components in healthy organs over time warrants systematic evaluation.
Moreover, the interaction of these complex nanoparticles with the immune system is not fully understood. There is a risk that they could inadvertently activate the complement system, a part of the innate immune response, leading to adverse inflammatory reactions. Oxidative stress–sensitive nanoparticles, in particular, may engage these pathways. Furthermore, in specific applications like bladder cancer therapy, potential entry into the bloodstream via compromised mucosal linings raises additional concerns about systemic exposure that must be addressed in more clinically relevant models.
Scaling Up and Clinical Feasibility
The practical obstacles to widespread clinical adoption are also substantial. The multi-step synthesis required to create these sophisticated, multi-component nanocarriers is often complex, time-consuming, and difficult to scale up to the quantities needed for clinical trials and commercial production while maintaining consistent quality. This manufacturing complexity presents a significant hurdle for regulatory approval.
Bridging the gap from promising preclinical data to successful patient care requires further validation. The targeting mechanisms need to be rigorously confirmed at the cellular and tissue levels in models that more closely mimic human physiology. Comprehensive long-term safety and efficacy studies are essential to build a strong case for clinical translation. Overcoming these hurdles will be critical to realizing the full potential of dual-responsive nanodelivery in the clinic.
Future Outlook and Next-Generation Systems
The trajectory for dual-responsive nanodelivery points toward even greater sophistication and personalization. Future breakthroughs are expected in the development of multi-responsive systems capable of sensing three or more distinct stimuli, allowing for unprecedented levels of precision in even more complex disease environments. This could involve integrating responses to biological cues with external triggers to create highly tunable therapeutic platforms.
Another exciting frontier is the fusion of therapy and diagnostics into single “theranostic” platforms. By incorporating imaging agents into the nanocarrier, clinicians could visualize tumor accumulation in real time, confirm on-target delivery, and monitor therapeutic response non-invasively. Furthermore, the application of artificial intelligence and machine learning is poised to revolutionize nanocarrier design. AI algorithms could rapidly screen vast libraries of materials and formulations to create optimized, patient-specific nanosystems tailored to an individual’s unique tumor biology, heralding a new era of personalized nanomedicine.
Concluding Remarks
Dual-responsive nanodelivery systems stand as a powerful and highly adaptable strategy for modern therapeutics. The ability of these platforms to navigate complex biological environments and execute precise, microenvironment-specific drug release has enabled the development of synergistic, multimodal therapies that were previously impractical. By co-delivering agents that target cancer cells directly while simultaneously reprogramming the tumor immune microenvironment, these systems have shown a remarkable capacity to overcome immunotherapy resistance and inhibit metastatic progression in challenging cancers. This work established not only a theoretical basis for enhancing therapeutic efficacy but also a firm technical foundation for developing the next wave of advanced, intelligent medicines.