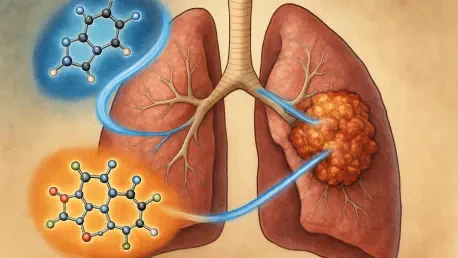
A formidable new strategy has emerged in the fight against a particularly stubborn form of lung cancer, offering a beacon of hope for patients whose tumors have developed resistance to frontline treatments. Researchers from the Medical University of Vienna have pioneered a novel combination therapy that successfully targets and dismantles lung adenocarcinomas driven by KRAS gene mutations, a common and aggressive subtype notorious for its ability to evade even the most advanced targeted drugs. This groundbreaking approach employs a dual-drug assault that exploits a critical vulnerability—an acquired “addiction” to secondary survival pathways—that cancer cells develop as they evolve. By simultaneously blocking two of these essential pathways, the therapy creates a synergistic effect that not only halts tumor growth but also triggers the complete elimination of resistant cancer cells in preclinical models, paving the way for a powerful new therapeutic option.
Unmasking the Tumor’s Achilles’ Heel
The central challenge in treating KRAS-mutated lung cancer is the tumor’s remarkable adaptability, as these cancers, which account for nearly a third of all lung adenocarcinomas, frequently render targeted therapies ineffective within months. Modern drugs like sotorasib, which specifically inhibits the KRAS-G12C mutation, represent a major step forward, but their benefits are often transient. Tumors cleverly circumvent these inhibitors by activating alternative signaling networks, creating bypass routes that allow them to continue their relentless growth and proliferation. However, this evolutionary sleight of hand is not a sign of invincibility. Instead, it forces the cancer cells into a state of dependency on these newly activated pathways. This acquired reliance, once hidden, becomes the tumor’s Achilles’ heel, presenting a unique and exploitable target for a more sophisticated therapeutic attack that can outmaneuver the cancer’s adaptive strategies and overcome its hard-won resistance.
Further investigation into this mechanism of resistance revealed that as tumors evade KRAS inhibition, they become critically dependent on two specific molecular systems to survive. The first is the ERBB family of receptor tyrosine kinases, a group of proteins on the cell surface that includes the well-known epidermal growth factor receptor (EGFR). These receptors act as antennas, receiving external growth-promoting signals and relaying them into the cell’s interior to drive division and proliferation. The second critical dependency is on Aurora kinases, a family of enzymes that serve as master regulators of mitosis. These kinases ensure the orderly and accurate segregation of genetic material into daughter cells during cell division, a process that is absolutely essential for tumor expansion. In resistant cancer cells, the ERBB and Aurora kinase pathways work in concert as a non-negotiable lifeline, sustaining the tumor’s survival and growth after the primary KRAS pathway has been therapeutically blocked, thereby creating a precise vulnerability for a dual-targeted intervention.
Crafting a Synergistic Combination
With these critical dependencies identified, researchers embarked on an extensive screening process to find active substances capable of disabling both survival pathways simultaneously. This methodical search revealed that a combination of the pan-ERBB inhibitor afatinib and an Aurora kinase inhibitor was exceptionally effective. Afatinib is a powerful, established drug that broadly blocks multiple members of the ERBB receptor family, providing a comprehensive shutdown of their growth-promoting signals. When paired with a compound designed to inhibit Aurora kinases, the therapy creates a devastating one-two punch. This synergistic strategy attacks the tumor from two distinct angles: it severs the external communication lines telling the cancer to grow while simultaneously sabotaging the internal machinery required for the cell to divide. This dual blockade effectively corners the cancer cells, leaving them with no viable route to sustain their proliferation or to evolve further resistance, a crucial advantage over single-agent therapies.
The efficacy of this dual-drug approach was rigorously validated in preclinical cell and mouse models of KRAS-mutated lung adenocarcinoma, where the results demonstrated a multifaceted and potent anti-cancer effect. The combination therapy did far more than simply slow tumor progression; it initiated a cascade of events that led to the systematic destruction of the cancer cells. Researchers observed a significant increase in apoptosis, or programmed cell death, a controlled process that cleanly eliminates malignant cells without triggering inflammation. At the same time, the inhibition of Aurora kinases brought cell division to a screeching halt, preventing the tumor from expanding. Critically, the dual blockade of both ERBB and Aurora kinase signaling effectively closed off the primary escape routes that tumors typically exploit to develop resistance. This comprehensive assault created a therapeutic dead-end for the cancer, resulting in the complete elimination of resistant cell clones within the experimental models.
A New Strategy for Treatment-Resistant Cancers
Perhaps the most profound discovery of the study is the combination’s remarkable effectiveness against tumors that had already developed resistance to existing state-of-the-art treatments. The dual-drug regimen of afatinib and an Aurora kinase inhibitor proved to be highly potent even in tumor models that had stopped responding to the targeted KRAS inhibitor sotorasib or to afatinib when used as a standalone therapy. This finding is of immense clinical significance, as it positions the combination as a powerful potential second-line or even third-line therapy for patients whose cancer has progressed following initial treatment regimens. The ability to successfully treat these highly evolved, treatment-refractory tumors addresses a major unmet need in oncology and offers a new therapeutic avenue for a patient population with increasingly limited options. The strategy effectively resets the board, turning the tumor’s own mechanism of resistance into its ultimate downfall.
The potent effect of this combination is rooted in a biological principle known as synthetic lethality, a scenario where the simultaneous disruption of two separate molecular pathways leads to cell death, whereas the disruption of either pathway alone does not. In the context of these resistant lung cancer cells, while they might be able to survive the inhibition of either the ERBB or the Aurora kinase pathway by compensating through other mechanisms, they are unable to withstand the dual assault. Blocking both pathways at the same time creates a catastrophic system failure from which the cancer cell cannot recover. This synthetic lethal interaction ensures that the cancer has no alternative survival strategy to fall back on, leading to a complete collapse of its cellular machinery. This robust mechanism explains why the combination was so effective at eradicating even the most stubborn, therapy-resistant cell clones, offering a blueprint for designing highly effective treatments against adaptive tumors.
Paving the Way for Clinical Application
The extensive preclinical research concluded with a very promising outlook for the eventual translation of these findings into clinical practice. A significant advantage that could expedite this journey from the laboratory to patient care was the advanced developmental status of the individual drugs used in the combination. Afatinib is already an established and approved medication widely used in oncology for its potent inhibition of the ERBB receptor family, meaning its safety profile and dosage are well understood. Furthermore, several Aurora kinase inhibitors are currently undergoing advanced clinical trials for various cancers, which has generated a substantial body of data regarding their use in humans. This existing foundation of clinical information could dramatically shorten the typical timeline required to design and launch clinical studies to evaluate this specific dual-drug combination in patients with KRAS-mutated lung cancer.
The study ultimately demonstrated a powerful proof of concept that shifted the paradigm for treating resistant cancers. By identifying and targeting the acquired vulnerabilities that tumors develop as they evolve, the research team established a strategic framework that could be applied to other difficult-to-treat cancers beyond just KRAS-mutated lung adenocarcinoma. The findings underscored the importance of moving beyond single-target therapies and toward more sophisticated, multi-pronged attacks that anticipate and exploit the very mechanisms of tumor adaptation. This work provided a robust preclinical foundation and a clear rationale for advancing this promising combination therapy into human trials, having successfully laid the groundwork for what could become a new standard of care for a patient population in dire need of more effective and durable treatment options.