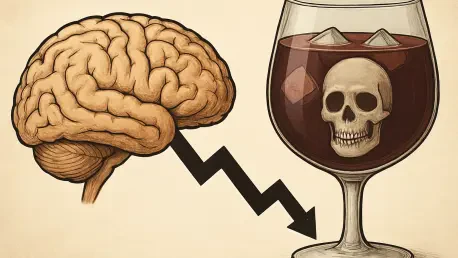
The intersection of alcohol consumption and brain health has long been a topic of debate, with past research suggesting that a glass of wine or a moderate drink might even offer protective benefits against cognitive decline. However, a groundbreaking study recently published in a leading medical journal has turned this notion on its head, revealing that any level of alcohol intake could heighten the risk of developing dementia. This extensive research, drawing from massive datasets and advanced genetic analysis, challenges decades of assumptions and raises critical questions about how society views alcohol’s role in long-term health. By examining data from hundreds of thousands of participants across diverse populations, the study provides a compelling case that there may be no safe threshold when it comes to drinking and brain health. This revelation not only reshapes scientific understanding but also prompts a reevaluation of public health guidelines surrounding alcohol use and its impact on aging populations.
Revisiting Old Assumptions About Alcohol and Brain Health
For years, the relationship between alcohol and dementia was framed by studies suggesting a U-shaped pattern, where moderate drinkers seemed to have a lower risk of cognitive decline compared to non-drinkers or heavy drinkers. This idea fueled the belief that small amounts of alcohol, such as a daily glass of red wine, might safeguard brain function through mechanisms like improved cardiovascular health. However, these earlier findings often relied on observational data with significant limitations, such as failing to account for whether non-drinkers were lifelong abstainers or former drinkers who stopped due to health issues. Such methodological flaws muddied the waters, making it difficult to establish whether alcohol truly offered any protective effect or if other factors were at play. The notion of an “optimal dose” became a widely accepted hypothesis, influencing both medical advice and personal habits, despite the lack of definitive proof.
The latest research, however, dismantles this long-standing narrative with a more robust approach, combining observational data with cutting-edge genetic analysis. Unlike prior studies that focused narrowly on aging populations, this comprehensive effort spans nearly 560,000 participants across varied age groups and backgrounds, tracked over extended periods. The findings starkly contrast with older assumptions, showing no evidence of a protective effect at any level of alcohol consumption. Instead, the data indicates a linear increase in dementia risk as alcohol intake rises, even among those who drink lightly. This shift in understanding underscores the importance of revisiting outdated beliefs with modern scientific tools, revealing that what was once considered a potential health benefit may, in fact, be a hidden risk factor for cognitive decline over time.
Unpacking the Latest Evidence on Alcohol’s Impact
Delving into the specifics of this landmark study, the observational data initially appears to echo past findings with a U-shaped association: non-drinkers and heavy drinkers (consuming 40 or more drinks weekly) showed a 41% higher dementia risk compared to light drinkers (fewer than 7 drinks per week). Yet, this pattern unravels under deeper scrutiny through genetic analysis involving over 2.4 million individuals. Using techniques like Mendelian randomization, which helps isolate causal relationships, the research found no protective curve. Instead, it revealed that even a modest increase of 1-3 drinks per week correlates with a 15% higher dementia risk. For those with a genetic predisposition to alcohol dependency, the risk escalates further, with a doubling of genetic markers linked to a 16% increase in likelihood. These results paint a clear picture that any alcohol consumption, regardless of quantity, contributes to heightened vulnerability.
Beyond the raw numbers, the study also addresses a critical flaw in earlier research known as reverse causation. It was observed that individuals who later developed dementia often reduced their drinking in the years preceding diagnosis, creating a false impression that light drinking was beneficial. This behavioral shift, likely influenced by early, undiagnosed cognitive decline, skewed past conclusions and highlights the complexity of studying alcohol’s long-term effects. The integration of genetic data in this analysis helps bypass such confounding factors, offering a clearer lens on causality. While the findings predominantly reflect participants of European ancestry, limiting broader applicability, they still provide a compelling argument against the idea of a safe drinking level. This nuanced perspective challenges both individuals and health professionals to rethink alcohol’s role in brain health strategies.
Implications for Public Health and Future Research
The implications of this research extend far beyond academic circles, carrying significant weight for public health policies and individual lifestyle choices. If no level of alcohol consumption can be deemed safe for brain health, as the study suggests, then current guidelines that permit moderate drinking may need urgent revision. Governments and health organizations worldwide could face pressure to lower recommended limits or advocate for complete abstinence as a preventive measure against dementia. This shift could influence everything from alcohol taxation to public awareness campaigns, emphasizing reduction over moderation. For individuals, the findings serve as a stark reminder that even occasional drinks might contribute to long-term cognitive risks, prompting a reassessment of personal habits in light of emerging science.
Looking ahead, the limitations of this study pave the way for critical next steps in research. Since the data primarily represents individuals of European descent, future studies must prioritize diverse populations to ensure findings are universally applicable. Additionally, addressing residual confounding factors in observational research remains a challenge, necessitating innovative methodologies to refine accuracy. Scientists and policymakers have already begun exploring these avenues, with plans to expand genetic studies and longitudinal tracking over the coming years. Reflecting on the past trajectory, it is evident that assumptions about alcohol’s benefits were overturned by rigorous analysis, setting a precedent for cautious interpretation. The journey forward involves a collective push to minimize alcohol intake as a viable dementia prevention strategy, ensuring that both individual choices and systemic policies align with the latest evidence for a healthier future.