In the ceaseless battle against cancer, a remarkable stride forward has surfaced, promising to reshape the landscape of treatment options for patients worldwide. Chimeric Antigen Receptor T-cell (CAR-T) therapy, a cutting-edge immunotherapy that reengineers a patient’s immune cells to seek out and destroy cancer, has already proven its worth in combating specific blood cancers like leukemia. Yet, its impact on solid tumors—such as those found in breast, lung, or pancreatic cancers—has been constrained by the intricate and varied nature of these growths. Now, researchers at St. Jude Children’s Research Hospital have unveiled a pioneering computational tool that optimizes CAR-T cell design, offering renewed hope for tackling these challenging cancers with greater precision and effectiveness.
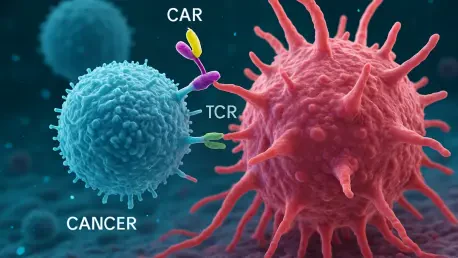
This innovation focuses on enhancing tandem bispecific CAR-T cells, which are uniquely engineered to target two distinct antigens on cancer cells simultaneously. By addressing the diverse antigen expression in solid tumors, this dual-targeting strategy seeks to eliminate a broader range of cancer cells, thereby reducing the likelihood of relapse. The computational tool streamlines what was once a labor-intensive process, marking a significant advancement in making CAR-T therapy more adaptable and potent against a wider array of cancers.
Tackling the Barriers of Solid Tumors
Addressing Tumor Complexity
Solid tumors present a formidable challenge in cancer treatment due to their heterogeneous nature, which often renders single-target therapies less effective. Unlike blood cancers, where CAR-T therapy has shown dramatic success by targeting a uniform antigen, solid tumors display a patchwork of antigens across their cells. This variability means that many cancer cells can evade attack, leading to incomplete treatment and a high risk of recurrence. The diversity within these tumors underscores the urgent need for a more comprehensive approach that can address multiple targets at once, ensuring that fewer cancer cells slip through the therapeutic net and improving long-term outcomes for patients facing these stubborn diseases.
The development of tandem bispecific CAR-T cells represents a strategic pivot toward overcoming this hurdle by enabling the simultaneous targeting of two antigens. This dual approach increases the likelihood of hitting a wider spectrum of cancer cells within a tumor, tackling the issue of antigen variability head-on. By enhancing the scope of attack, researchers aim to curtail the chances of relapse, offering a potential lifeline to those with solid tumors who have limited options with conventional treatments. This shift in strategy is a critical step toward making CAR-T therapy a viable solution for a broader patient population.
Navigating Treatment Resistance
Beyond antigen diversity, solid tumors often create a hostile microenvironment that suppresses immune responses, adding another layer of difficulty to effective treatment. This environment can hinder the activity of CAR-T cells, reducing their ability to infiltrate and destroy cancer cells. The resistance posed by such conditions necessitates innovative designs that not only target multiple antigens but also bolster the resilience of modified T-cells against these suppressive mechanisms. Addressing this challenge is vital to unlocking the full potential of CAR-T therapy in solid tumor contexts.
Efforts to counter this resistance are bolstered by the computational tool’s ability to predict and optimize CAR-T cell performance under varied conditions. By simulating interactions within the tumor microenvironment, the tool helps identify designs that can withstand immune suppression while maintaining robust anti-tumor activity. This predictive capacity ensures that the engineered cells are not only diverse in their targeting but also hardy enough to function in challenging settings, paving the way for therapies that can penetrate deeper into the complexities of solid tumors and deliver lasting impact.
Revolutionizing CAR-T Design with Technology
Accelerating Development Through Computation
Designing tandem bispecific CAR-T cells has historically been a daunting task, marked by extensive trial and error that consumes significant time and resources. Each potential construct required laborious testing to assess its surface expression on T-cells and its effectiveness against cancer cells, often leading to delays in therapeutic advancement. The introduction of a novel computational tool by researchers at St. Jude Children’s Research Hospital transforms this process by automating the evaluation of countless theoretical designs. This innovation slashes development timelines, enabling scientists to focus on the most promising candidates for further exploration and bringing effective treatments closer to clinical application.
The efficiency brought by this tool is underpinned by its use of artificial intelligence and machine learning to analyze vast datasets and predict outcomes with remarkable accuracy. By modeling how different CAR constructs might perform, including their ability to bind to antigens and express on T-cell surfaces, the tool identifies optimal designs before any physical testing begins. This predictive power not only saves resources but also enhances the precision of CAR-T therapy development, ensuring that the resulting cells are tailored for maximum impact against specific cancer profiles. Such technological integration marks a turning point in how therapies are crafted for complex diseases.
Enhancing Precision in Therapy Customization
The computational tool’s ability to refine CAR-T cell design extends beyond mere speed, delving into the realm of personalized medicine where treatments are customized to individual patient needs. By simulating molecular interactions and forecasting anti-tumor activity, the tool helps pinpoint constructs that align with the unique characteristics of a patient’s cancer. This level of customization is crucial for addressing the variability seen in solid tumors, where a one-size-fits-all approach often falls short. The result is a therapy that can be fine-tuned to target specific antigen combinations, potentially improving efficacy and reducing unintended side effects.
Moreover, preclinical studies have validated the tool’s predictions, demonstrating that optimized tandem CAR-T cells outperform their single-target counterparts in both surface expression and tumor-fighting capability. These findings, as highlighted by Dr. Giedre Krenciute, a key researcher in the study, fuel optimism about the tool’s potential to redefine CAR-T therapy’s reach. The ability to craft highly specific and effective cells through computational guidance aligns with the broader movement toward precision oncology, where treatments are increasingly designed to match the genetic and molecular nuances of each patient’s disease, promising better outcomes.
Envisioning the Future of Cancer Care
Broadening the Scope of CAR-T Applications
The implications of this computational breakthrough are profound, potentially expanding CAR-T therapy’s applicability to a wider range of cancers that currently lack effective treatment options. By enhancing the design of tandem bispecific CAR-T cells, this innovation offers new hope to patients with solid tumors, where traditional therapies often fail to provide lasting remission. The ability to target multiple antigens simultaneously addresses a critical gap in current approaches, suggesting a future where even the most resistant cancers might be managed more effectively. This progress could significantly alter the therapeutic landscape, bringing renewed possibilities to countless individuals.
As research progresses, upcoming clinical trials will be pivotal in assessing the safety and efficacy of these optimized CAR-T cells in human patients. These trials will provide crucial data on how well the computationally designed cells perform in real-world scenarios, particularly against solid tumors. Additionally, exploring combination strategies with other treatments, such as checkpoint inhibitors, could further enhance outcomes by tackling multiple barriers to effective cancer control. The potential to integrate CAR-T therapy into broader treatment regimens highlights its evolving role in comprehensive cancer care.
Pioneering a New Era of Medical Innovation
Reflecting on the strides made, this computational advancement in CAR-T therapy stands as a testament to the power of merging technology with medical science. The collaboration between computational experts, immunologists, and oncologists yielded a tool that redefined how therapies are developed, setting a precedent for future innovations. The preclinical successes of optimized tandem CAR-T cells underscored a turning point, where data-driven design became integral to overcoming cancer’s complexities. Looking back, the integration of artificial intelligence into therapy development marked a historic shift toward precision and efficiency in addressing some of the most challenging diseases.
Moving forward, the focus should center on scaling these innovations through rigorous clinical testing and broader interdisciplinary partnerships. Exploring how this computational approach can be applied to other areas of medicine, beyond CAR-T therapy, could unlock further breakthroughs in personalized treatment. Additionally, addressing the cost and accessibility of such advanced therapies remains critical to ensuring that the benefits reach a diverse patient population. As the synergy between technology and healthcare continues to deepen, the path ahead promises to build on these achievements, driving toward a future where cancer treatment is not only more effective but also universally attainable.