I’m thrilled to sit down with Dr. Ivan Kairatov, a renowned interventional cardiologist and senior scientist at the Population Health Research Institute. With his extensive expertise in heart attack treatment strategies, Dr. Kairatov has been at the forefront of groundbreaking research on complete revascularization, a game-changing approach for patients suffering from heart attacks. In this conversation, we dive into the findings of a major international study he led, exploring how treating all blocked arteries can save lives, the implications for patient care, and what this means for the future of cardiology.
Can you explain what complete revascularization means for someone who might not be familiar with the term?
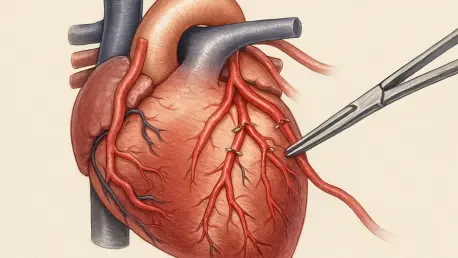
Absolutely. Complete revascularization refers to a procedure where we open up all significantly blocked arteries in a patient’s heart using stents, not just the one directly causing the heart attack, which we call the culprit artery. Think of it as clearing all the major roadblocks in a traffic system, not just the one causing the immediate crash. This approach aims to restore blood flow throughout the heart to prevent further damage or future issues.
How does this differ from the more traditional method of treating only the culprit artery?
The traditional method focuses solely on the culprit artery—the one responsible for the heart attack. We’d go in, place a stent, and restore blood flow to that specific area. While this can be effective in the short term, it leaves other blocked or narrowed arteries untreated, which could still pose risks down the line. Complete revascularization takes a broader view, addressing all major blockages to improve overall heart function and reduce long-term complications.
What sparked the idea for this large international study on complete revascularization?
We’ve known for a while that treating just the culprit artery might not be enough for some patients, especially those with multiple blockages. Earlier studies hinted that complete revascularization could reduce non-fatal heart events, but there was a big question mark around whether it actually lowered the risk of death from heart-related causes. That uncertainty drove us to pool data from multiple trials worldwide to get a clearer, more definitive answer on this critical outcome.
Can you walk us through the most significant findings from your study published in The Lancet?
Certainly. Our study, which looked at over 8,000 patients across six international trials, showed that complete revascularization significantly cuts down the risk of death from cardiovascular causes by about 24%. It also reduced overall death rates by 15% and lowered the chances of future heart attacks. Over a three-year follow-up, only 9% of patients with complete revascularization experienced a cardiovascular death or new heart attack, compared to 11.5% in the group where only the culprit artery was treated. These numbers highlight a real, life-saving impact.
How did you manage to ensure the reliability of data with such a diverse group of patients from different countries?
That was a challenge, but we tackled it by sticking to rigorous standards across all trials. We combined individual patient data from each study, which allowed us to analyze outcomes consistently, regardless of location. We also worked closely with trial coordinators to harmonize how data was collected and reported. While there were logistical hurdles, like differences in healthcare systems, our focus on standardized endpoints—such as cardiovascular death or new heart attacks—helped ensure the results were trustworthy.
Your research covered both STEMI and NSTEMI heart attacks. Could you break down what these terms mean for our audience?
Of course. STEMI stands for ST-segment elevation myocardial infarction, which is often called a full-blown heart attack. It happens when an artery is completely blocked, cutting off blood flow to a large part of the heart muscle. NSTEMI, or non-ST-segment elevation myocardial infarction, is a smaller heart attack caused by a severe but partial blockage, so the damage might be less immediate but still serious. Both are critical, just different in severity and how they show up on heart tests.
Did complete revascularization prove equally effective for both types of heart attacks?
Yes, one of the encouraging findings was that complete revascularization benefited patients with both STEMI and NSTEMI. Regardless of whether the blockage was total or partial, opening all significant blockages reduced the risk of death and future events. This broad effectiveness suggests the approach isn’t limited to one specific type of heart attack, which is huge for tailoring treatment plans.
How do you see these findings influencing the way doctors treat heart attack patients moving forward?
I believe this study provides strong evidence to shift toward complete revascularization as a preferred strategy for many patients with multiple blockages. It’s not just about preventing future heart attacks anymore—it’s about prolonging life. That said, it won’t be a one-size-fits-all solution. Some patients might still do better with a more focused approach due to factors like overall health or procedural risks. But for most, this could become the new benchmark.
What can you tell us about the long-term benefits for patients who underwent complete revascularization compared to those who didn’t?
Over the three-year follow-up in our study, patients who had complete revascularization consistently showed better outcomes. They had a lower rate of cardiovascular death—3.6% versus 4.6%—and fewer new heart attacks compared to those who only had the culprit artery treated. Even all-cause mortality was reduced, which means we’re not just addressing heart issues but improving overall survival. It’s a powerful testament to how clearing all blockages can protect the heart in the long run.
What is your forecast for the future of heart attack treatment based on these results?
I’m optimistic that we’ll see complete revascularization become more widely adopted as technology and techniques continue to improve, making the procedure safer and more accessible. I also think we’ll see more research into personalizing this approach—figuring out exactly which patients benefit most and refining how we assess blockages. Beyond that, integrating this strategy with advances in medications and lifestyle interventions could transform heart attack care, pushing survival rates even higher in the coming years.