Imagine a world where a single treatment could halt the relentless cycle of relapse in a disease as challenging as multiple myeloma, a blood cancer notorious for its grim prognosis in advanced stages, offering hope to patients who have exhausted standard therapies. For these patients, the outlook has often been bleak, marked by repeated setbacks and diminishing hope. Yet, a groundbreaking advancement in cellular immunotherapy, specifically ciltacabtagene autoleucel (cilta-cel), is rewriting this narrative. This CAR T-cell therapy has shown remarkable potential to deliver long-term remission and significantly extend survival, even in heavily pretreated cases. By harnessing the body’s own immune system to target cancer cells with precision, this innovative approach offers a beacon of hope for those facing relapsed or refractory multiple myeloma. The impact of such a therapy cannot be overstated, as it challenges the historical limitations of treatment and sets a new standard for what is possible in managing this complex hematologic malignancy.
A Breakthrough in Cellular Immunotherapy
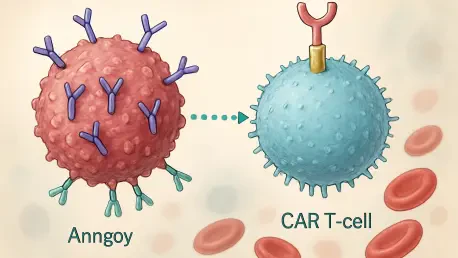
The emergence of cilta-cel as a transformative option for multiple myeloma patients represents a significant leap forward in the field of oncology. This CAR T-cell therapy involves modifying a patient’s T cells to recognize and attack myeloma cells, a process that culminates in a single infusion following lymphodepletion to enhance effectiveness. Studies tracking outcomes over an extended period have revealed stunning results, with nearly half of the participants surviving beyond five years post-treatment. This is a stark contrast to the historical expectation of less than a year for similar patient groups. Moreover, about one-third of these individuals remained in remission at the five-year mark, many with no detectable signs of disease. Such durability of response underscores the potential of this therapy to alter the disease trajectory fundamentally, offering not just temporary relief but a sustained reprieve from the burdens of multiple myeloma.
Beyond the impressive survival statistics, the therapy’s ability to maintain remission over time is a testament to its innovative design. Median overall survival has exceeded five years, while progression-free survival approaches four years, numbers that were once unimaginable for patients with relapsed or refractory disease. Importantly, the benefits of cilta-cel appear to extend across a diverse patient population, including older adults and those with high-risk features or numerous prior treatments. This broad applicability suggests that the therapy is not limited to a niche group but could serve a wide array of individuals battling this cancer. While the results are undeniably promising, the medical community continues to grapple with understanding why some patients still experience relapse, highlighting the need for ongoing research to refine and optimize this cutting-edge treatment for even greater impact.
Safety and Manageability of Treatment Challenges
While the efficacy of cilta-cel is remarkable, addressing the safety profile is equally critical to its adoption in clinical practice. Patients undergoing this therapy often encounter side effects such as cytokine release syndrome (CRS) and neurological toxicities, which can manifest as confusion or tremors. However, data from long-term follow-ups indicate that these adverse events typically occur early in the treatment course and are generally manageable with appropriate medical intervention. Most importantly, these issues tend to resolve without leaving lasting impacts on patient health. The absence of new safety concerns over extended observation periods further bolsters confidence in the therapy’s risk-benefit profile, suggesting that with proper care, the challenges associated with cilta-cel can be effectively navigated.
Equally reassuring is the structured approach to monitoring and mitigating these side effects, ensuring patient safety remains a priority. Medical teams have developed protocols to address CRS and neurological symptoms promptly, minimizing discomfort and potential complications. This focus on manageable care is vital for patients who, having exhausted other options, may already face significant health burdens. The ability to handle these acute challenges without compromising long-term outcomes speaks to the robustness of the therapy’s framework. Nevertheless, continuous vigilance is necessary to adapt to any evolving safety considerations as more patients gain access to this treatment. As the therapy becomes more widely implemented, refining these supportive measures will be essential to maintaining trust and efficacy in real-world settings.
Future Horizons in Myeloma Care
Looking ahead, the success of cilta-cel paves the way for broader implications in the management of multiple myeloma, though it is not without its limitations. While the therapy has achieved unprecedented remission rates, relapses in some cases signal the need for deeper insights into predicting treatment responses. Developing reliable biomarkers could help identify which patients are most likely to benefit, tailoring the approach for maximum impact. Additionally, exploring combination strategies with other therapies might enhance the durability of remission, addressing the gaps where disease progression persists. These avenues of research hold the promise of further elevating the standard of care for a condition that has long defied lasting solutions.
Reflecting on the strides made, it is evident that the journey with cilta-cel marks a turning point in redefining expectations for advanced multiple myeloma treatment. The focus now shifts to actionable steps, such as integrating this therapy into earlier lines of care and expanding access to more patients globally. Collaborative efforts among researchers, clinicians, and industry stakeholders will be crucial to overcoming remaining hurdles and ensuring that the benefits witnessed in clinical studies translate to diverse real-world populations. By building on this foundation, the medical field can continue to innovate, striving toward a future where sustained remission becomes the norm rather than the exception for those battling this formidable disease.