A baffling contradiction has long stood at the heart of understanding how one of the most aggressive forms of breast cancer spreads throughout the body, but new research has finally unraveled this mystery, revealing a unique survival strategy that cancer cells use to become metastatic. For years, scientists struggled to explain how triple-negative breast cancer (TNBC) cells could form the deadly clusters essential for metastasis when they often lack the very proteins that typically glue cells together. This groundbreaking work not only solves that puzzle but also illuminates a promising new target for therapies aimed at stopping cancer’s fatal journey. The investigation clarifies how these cells compensate for their lack of traditional adhesion molecules, adopting an entirely different mechanism to stick together and enhance their ability to seed new tumors in distant organs.
Unraveling a Metastatic Paradox in Aggressive Breast Cancer
The journey of cancer from a primary tumor to other parts of the body, a process known as metastasis, is significantly more successful when cancer cells travel in groups. These circulating tumor cell (CTC) clusters are better equipped to survive the harsh environment of the bloodstream and are more efficient at establishing new tumors than individual cells. This understanding formed the basis of a perplexing scientific question surrounding triple-negative breast cancer. While the principle of cluster-based metastasis is well-established, the mechanics behind it were thought to rely heavily on a family of proteins called adherens junctions (AJs), which serve as a biological cement, holding cells together in a stable formation.
This established model, however, did not align with observations in TNBC. This particularly aggressive cancer is characterized by the loss of these very AJ proteins, a feature that should, in theory, make it difficult for its cells to form resilient clusters. This contradiction presented a major challenge to researchers: if TNBC cells lack the standard “glue,” how do they manage to form the highly metastatic clusters that make the disease so dangerous? The research delved into this paradox, seeking to identify the alternative adhesion strategy that these cancer cells employ to achieve their deadly cohesiveness and drive the metastatic cascade.
The Critical Need for New Metastatic Insights
Metastasis remains the primary cause of nearly all cancer-related deaths, yet the intricate mechanisms that govern it are still not fully understood. Progress in this area is paramount to improving patient outcomes, as stopping the spread of cancer is as critical as treating the primary tumor. Research that uncovers the fundamental processes driving metastasis provides the scientific community with the essential knowledge needed to design more effective and targeted interventions. Without a deep understanding of how cancer cells adapt, survive, and colonize new territories, therapeutic strategies remain limited in their ability to halt the disease’s progression.
This need is especially urgent in the context of triple-negative breast cancer. TNBC is notorious for its aggressive behavior, rapid progression, and high rates of recurrence. Unlike other types of breast cancer, it lacks the three common receptors—estrogen, progesterone, and HER2—that are the targets of many successful hormonal and targeted therapies. This leaves patients with fewer treatment options, primarily limited to conventional chemotherapy. Discovering the unique mechanism by which TNBC cells cluster and spread, therefore, represents more than a scientific curiosity; it offers a critical opportunity to develop a novel class of therapies specifically for a patient population in desperate need of new hope.
Research Methodology, Findings, and Implications
Methodology
To dissect this complex biological puzzle, researchers employed a multi-faceted approach centered on comparative analysis. The investigation began by meticulously comparing the molecular and cellular characteristics of TNBC cells with non-TNBC cells, as well as contrasting metastatic breast cancers with their non-metastatic counterparts. This systematic comparison allowed the team to pinpoint the distinct biological properties associated with the highly metastatic phenotype, guiding them toward the unconventional adhesion mechanism at play.
The study’s scope extended beyond cell cultures to incorporate more complex biological systems that better mimic human disease. Mouse models were utilized to observe the entire metastatic process in a living organism, providing invaluable insights into how tumor cells form clusters, travel through the bloodstream, and seed new growths in real-time. Complementing these preclinical models, the research team analyzed blood samples from patients with breast cancer. This crucial step involved isolating and examining naturally occurring CTC clusters, ensuring that the findings were directly relevant to the human condition and confirming that the identified mechanisms were active in patients.
Findings
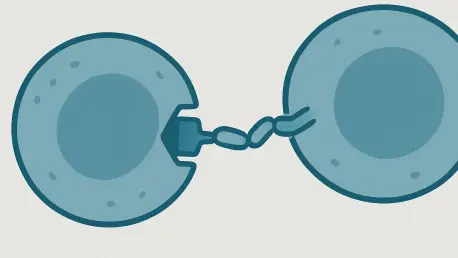
The comprehensive investigation led to a pivotal discovery: metastatic TNBC cells manufacture their own adhesive by enveloping themselves in a “sticky coat” made of a specific carbohydrate called hyaluronan (HA). The study revealed that these cells dramatically overproduce this substance using an enzyme called HAS2, which was found in exceptionally high levels. This HA coat functions as the primary adhesive, enabling the cells to cling to one another. When researchers experimentally removed this coat, the CTC clusters promptly disintegrated, confirming HA’s central role in maintaining cluster integrity.
Further analysis uncovered that this mechanism is a finely tuned molecular partnership. The sticky HA coat is not effective on its own; it requires a specific docking point on the cell surface, a protein known as CD44. HA must bind to CD44 to anchor itself to the cell, and this interaction is further reinforced by a set of proteins called desmosomes that add structural stability. This HA-CD44 axis creates uniquely flexible and resilient clusters. This pliability allows the clusters to deform and squeeze through the body’s narrowest blood vessels—a major physical barrier to metastasis—and then reassemble on the other side. Moreover, the HA coat also acts as a trap for protective immune cells, such as neutrophils, which naturally express CD44 and are captured by the cluster, shielding it from destruction.
Implications
The identification of the HA-CD44 adhesion axis as a key driver of metastasis in TNBC presents a clear and promising new target for therapeutic intervention. This discovery shifts the focus away from traditional cancer targets and opens the door to developing drugs that can specifically disrupt this interaction. Such therapies could be designed to either block the binding between HA and CD44, thereby preventing the formation of CTC clusters from the outset, or to break apart existing clusters already circulating in the bloodstream. By dismantling these metastatic seeds, it may be possible to significantly inhibit the spread of cancer to distant organs.
The potential impact of this research may extend far beyond breast cancer. Preliminary evidence gathered during the study suggests that a similar HA-CD44-mediated clustering mechanism is also active in other highly aggressive cancers, including glioblastoma, prostate, and pancreatic cancer. This finding raises the exciting possibility that a therapeutic strategy targeting this axis could have broad applications across multiple cancer types. If this mechanism is confirmed to be a common pathway for metastasis, a single class of drugs could potentially benefit a wide range of patients battling advanced cancers, representing a significant advancement in oncology.
Reflection and Future Directions
Reflection
This study provided a definitive resolution to the long-standing contradiction of how aggressive TNBC cells form cohesive, metastatic clusters in the absence of the typical adhesion molecules. By seamlessly integrating molecular biology, in-vivo animal models, and direct analysis of patient-derived cells, the researchers constructed a comprehensive and convincing explanation. The work demonstrated not just what holds these cells together, but also illuminated the functional advantages conferred by this unique adhesion system, offering a complete picture of a critical metastatic pathway.
The research made a substantial contribution by detailing the multifaceted benefits of the HA-CD44 clustering mechanism. It successfully explained how these clusters gain the physical flexibility needed to navigate the circulatory system’s narrow passages—a key logistical challenge for metastasis. Furthermore, it uncovered the clever strategy by which these cancer clusters co-opt the body’s own immune cells for protection. This comprehensive insight into the physical and biological superiority of HA-mediated clusters clarifies why they are such potent drivers of metastasis.
Future Directions
The immediate focus of future research will be on the development and rigorous testing of therapeutic agents designed to specifically inhibit the HA-CD44 interaction. This will involve screening for and designing molecules that can effectively block this binding process in preclinical models, with the ultimate goal of translating these findings into clinical trials for patients with metastatic cancer. Such work will be crucial in determining whether targeting this pathway can effectively prevent or treat metastasis in a clinical setting.
In parallel, further investigation is necessary to fully understand the prevalence and importance of this clustering mechanism across a wider spectrum of cancers. Expanding the research to include more cancer types will help determine how broadly a therapeutic strategy targeting the HA-CD44 axis could be applied. Validating this mechanism as a common feature in other aggressive malignancies would significantly strengthen the rationale for developing these novel anti-metastatic therapies and could ultimately transform the standard of care for many patients with advanced disease.
A New Target in the Fight Against Cancer’s Spread
This research fundamentally reshaped the scientific understanding of TNBC metastasis by uncovering a novel “sticky coat” mechanism that had previously been overlooked. The study identified the interaction between hyaluronan and the CD44 protein as the central axis enabling aggressive cancer cells to form deadly clusters capable of spreading throughout the body. By pinpointing this process as a critical driver of cancer’s progression, this work provided a major contribution to the field of oncology. The findings illuminated a clear, actionable target, laying the groundwork for the development of a next-generation class of anti-metastatic therapies designed to stop cancer in its tracks.