A new frontier is opening in the fight against cancer and other complex diseases, one that moves beyond the conventional strategy of simply destroying malignant cells and toward the more sophisticated approach of actively reprogramming them. In a significant leap forward for protein therapy, an interdisciplinary research team has developed two groundbreaking platform technologies that offer unprecedented control over the proteins displayed on a cell’s surface. These complementary methods provide distinct ways to intervene at the cellular level: one approach can selectively identify and destroy specific cancer-causing proteins, while the other can effectively repair a diseased cell by installing new, fully functional proteins, compelling it to return to a healthy state. This work addresses a long-standing challenge in cellular therapeutics and heralds a new era of highly customizable, precise medical interventions.
Decoding the Cell’s Surface
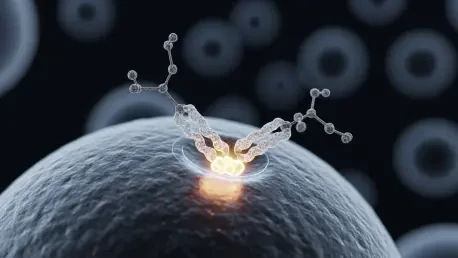
To appreciate this breakthrough, it is essential to move past the traditional, simplified view of a cell as a mere sac of organelles and instead recognize it as a complex, dynamic entity whose outer wall—the cell membrane—is a critical interface. This membrane is studded with thousands of different types of proteins that extend from the cell’s surface and perform vital functions, most notably maintaining a constant and intricate signaling pathway between the cell’s interior and its external environment. These proteins act as the cell’s gatekeepers, sensors, and communicators, managing everything from nutrient uptake to immune recognition. The sheer density and diversity of these proteins make the cell surface a bustling hub of biological activity, and its proper function is paramount to the health of the entire organism. This intricate protein landscape is the key to understanding both how diseases like cancer arise and how they can be defeated.
The research is built upon the fundamental understanding that when these crucial membrane proteins become damaged or defective, they can trigger catastrophic cellular behavior, leading to a host of diseases. For instance, a single faulty protein can erroneously and perpetually signal a cell to divide and grow without restraint, which is a hallmark of cancer. Furthermore, these defective proteins can act as a molecular “mask,” effectively camouflaging a malignant cell and allowing it to evade detection and destruction by the body’s own immune system. The strategic importance of these proteins is underscored by the fact that while they constitute only about 25% of the body’s more than 20,000 protein types, they are the target of approximately half of all modern pharmaceutical drugs. This research represents a significant evolution in therapeutic strategy, shifting the focus toward creating flexible, versatile platforms that leverage the cell’s own functions for more efficient and effective disease treatment.
Targeting and Eliminating Rogue Proteins
The first of these innovative platforms, named the Polymeric Lysosome-targeting Chimera, or PolyTAC, is engineered for a highly specific “search and destroy” mission. Its primary objective is to identify a single type of damage-causing protein on a cancer cell’s surface and then cleverly trick the cell into eliminating it. This technique represents a paradigm shift from traditional biochemical methods of protein removal to a novel physical mechanism. The team discovered that by physically pressing on a precise location on the cell membrane to create a small “dimple,” they could trigger the cell’s own internalization machinery. This physical deformation acts as a powerful signal, causing the cell to engulf the targeted surface protein and route it to its internal waste disposal system, the lysosome, where it is broken down and effectively “shredded.” This process neutralizes the cancerous threat posed by the protein without the need for harsh chemicals.
The PolyTAC platform itself is a sophisticated, two-part construct designed to execute this physical indentation with extreme specificity, ensuring that only the intended target is affected. The first component is an antibody, which functions as a highly specific targeting system. This antibody is carefully chosen to recognize and bind exclusively to the unique biomarker—akin to a molecular fingerprint—of the specific problem-causing protein on the cancer cell. This ensures the PolyTAC only acts on the intended cellular target. Once the antibody has guided the PolyTAC to the correct protein, the second component, a specialized polymer, comes into play. It is engineered to physically press into the cell membrane at the base of the targeted protein, creating the crucial dimple that initiates the cell’s natural disposal response. In practice, the antibody directs the platform, the polymer creates the physical trigger, and the cell’s own machinery completes the task of destroying the cancerous protein.
Repairing and Reprogramming from the Outside In
While the PolyTAC platform is designed to eliminate problematic proteins, the second platform offers a constructive and complementary alternative: repairing a cell by adding new, fully functional proteins to its surface. Developed by another team of researchers, this platform is called an Artificial Cell-derived Vesicle, or ACDV. Its primary function is to essentially reprogram a cancerous cell, compelling it to abandon its pathological behavior and return to its normal, healthy state. The ACDV technology allows researchers to directly fix cellular deficiencies by delivering and implanting fully functional proteins onto the cell membrane in real time. This capability opens the door to highly personalized and flexible therapies that can be tailored to the specific needs of an individual patient’s disease, moving beyond a one-size-fits-all approach to treatment.
This “repair and replace” strategy has profound therapeutic implications. For example, researchers can use the ACDV to introduce proteins that “unmask” a cancer cell, stripping away its molecular camouflage so that the body’s immune system can recognize and attack it. Alternatively, they can implant proteins that restore normal cell-cycle regulation, thereby halting pathological division and tumor growth. The team successfully demonstrated the platform’s efficacy by implanting four different types of functional proteins into a cell’s membrane, proving its versatility. They believe that with minor chemical modifications, this technique could be adapted to deliver a wide range of therapeutic proteins that are already on the market. The profound advantage of the ACDV method is that it moves beyond simply eliminating damaged components and instead enables the proactive incorporation of perfectly functional ones, fundamentally altering the cell’s behavior for the better.
A New Era of Cellular Customization
Ultimately, the development of these two distinct yet complementary platforms provided a powerful new toolkit for the field of cellular engineering. By creating reliable methods to both remove harmful proteins with the PolyTAC system and add beneficial ones with the ACDV system, this research established a new paradigm for intervention. The ability to transform the display of proteins on a cell’s surface made it possible to custom-tailor the way a cell functions, offering unprecedented control over its behavior. These avenues of research, which received support from major national health and science institutes, represented a significant advancement in the field of protein therapy. The work successfully moved the needle from generalized biochemical treatments toward precise, customizable interventions that could harness a cell’s own biological machinery to fight disease from within. The consensus was that these platform technologies held vast potential to be adapted for a wide range of immunological and cellular diseases, heralding a new era of personalized medicine.Fixed version:
A new frontier is opening in the fight against cancer and other complex diseases, one that moves beyond the conventional strategy of simply destroying malignant cells and toward the more sophisticated approach of actively reprogramming them. In a significant leap forward for protein therapy, an interdisciplinary research team has developed two groundbreaking platform technologies that offer unprecedented control over the proteins displayed on a cell’s surface. These complementary methods provide distinct ways to intervene at the cellular level: one approach can selectively identify and destroy specific cancer-causing proteins, while the other can effectively repair a diseased cell by installing new, fully functional proteins, compelling it to return to a healthy state. This work addresses a long-standing challenge in cellular therapeutics and heralds a new era of highly customizable, precise medical interventions.
Decoding the Cell’s Surface
To appreciate this breakthrough, it is essential to move past the traditional, simplified view of a cell as a mere sac of organelles and instead recognize it as a complex, dynamic entity whose outer wall—the cell membrane—is a critical interface. This membrane is studded with thousands of different types of proteins that extend from the cell’s surface and perform vital functions, most notably maintaining a constant and intricate signaling pathway between the cell’s interior and its external environment. These proteins act as the cell’s gatekeepers, sensors, and communicators, managing everything from nutrient uptake to immune recognition. The sheer density and diversity of these proteins make the cell surface a bustling hub of biological activity, and its proper function is paramount to the health of the entire organism. This intricate protein landscape is the key to understanding both how diseases like cancer arise and how they can be defeated.
The research is built upon the fundamental understanding that when these crucial membrane proteins become damaged or defective, they can trigger catastrophic cellular behavior, leading to a host of diseases. For instance, a single faulty protein can erroneously and perpetually signal a cell to divide and grow without restraint, which is a hallmark of cancer. Furthermore, these defective proteins can act as a molecular “mask,” effectively camouflaging a malignant cell and allowing it to evade detection and destruction by the body’s own immune system. The strategic importance of these proteins is underscored by the fact that while they constitute only about 25% of the body’s more than 20,000 protein types, they are the target of approximately half of all modern pharmaceutical drugs. This research represents a significant evolution in therapeutic strategy, shifting the focus toward creating flexible, versatile platforms that leverage the cell’s own functions for more efficient and effective disease treatment.
Targeting and Eliminating Rogue Proteins
The first of these innovative platforms, named the Polymeric Lysosome-targeting Chimera, or PolyTAC, is engineered for a highly specific “search and destroy” mission. Its primary objective is to identify a single type of damage-causing protein on a cancer cell’s surface and then cleverly trick the cell into eliminating it. This technique represents a paradigm shift from traditional biochemical methods of protein removal to a novel physical mechanism. The team discovered that by physically pressing on a precise location on the cell membrane to create a small “dimple,” they could trigger the cell’s own internalization machinery. This physical deformation acts as a powerful signal, causing the cell to engulf the targeted surface protein and route it to its internal waste disposal system, the lysosome, where it is broken down and effectively “shredded.” This process neutralizes the cancerous threat posed by the protein without the need for harsh chemicals.
The PolyTAC platform itself is a sophisticated, two-part construct designed to execute this physical indentation with extreme specificity, ensuring that only the intended target is affected. The first component is an antibody, which functions as a highly specific targeting system. This antibody is carefully chosen to recognize and bind exclusively to the unique biomarker—akin to a molecular fingerprint—of the specific problem-causing protein on the cancer cell. This ensures the PolyTAC only acts on the intended cellular target. Once the antibody has guided the PolyTAC to the correct protein, the second component, a specialized polymer, comes into play. It is engineered to physically press into the cell membrane at the base of the targeted protein, creating the crucial dimple that initiates the cell’s natural disposal response. In practice, the antibody directs the platform, the polymer creates the physical trigger, and the cell’s own machinery completes the task of destroying the cancerous protein.
Repairing and Reprogramming from the Outside In
While the PolyTAC platform is designed to eliminate problematic proteins, the second platform offers a constructive and complementary alternative: repairing a cell by adding new, fully functional proteins to its surface. Developed by another team of researchers, this platform is called an Artificial Cell-derived Vesicle, or ACDV. Its primary function is to essentially reprogram a cancerous cell, compelling it to abandon its pathological behavior and return to its normal, healthy state. The ACDV technology allows researchers to directly fix cellular deficiencies by delivering and implanting fully functional proteins onto the cell membrane in real time. This capability opens the door to highly personalized and flexible therapies that can be tailored to the specific needs of an individual patient’s disease, moving beyond a one-size-fits-all approach to treatment.
This “repair and replace” strategy has profound therapeutic implications. For example, researchers can use the ACDV to introduce proteins that “unmask” a cancer cell, stripping away its molecular camouflage so that the body’s immune system can recognize and attack it. Alternatively, they can implant proteins that restore normal cell-cycle regulation, thereby halting pathological division and tumor growth. The team successfully demonstrated the platform’s efficacy by implanting four different types of functional proteins into a cell’s membrane, proving its versatility. They believe that with minor chemical modifications, this technique could be adapted to deliver a wide range of therapeutic proteins that are already on the market. The profound advantage of the ACDV method is that it moves beyond simply eliminating damaged components and instead enables the proactive incorporation of perfectly functional ones, fundamentally altering the cell’s behavior for the better.
A New Era of Cellular Customization
Ultimately, the development of these two distinct yet complementary platforms provided a powerful new toolkit for the field of cellular engineering. By creating reliable methods to both remove harmful proteins with the PolyTAC system and add beneficial ones with the ACDV system, this research established a new paradigm for intervention. The ability to transform the display of proteins on a cell’s surface made it possible to custom-tailor the way a cell functions, offering unprecedented control over its behavior. These avenues of research, which received support from major national health and science institutes, represented a significant advancement in the field of protein therapy. The work successfully moved the needle from generalized biochemical treatments toward precise, customizable interventions that could harness a cell’s own biological machinery to fight disease from within. The consensus was that these platform technologies held vast potential to be adapted for a wide range of immunological and cellular diseases, heralding a new era of personalized medicine.