What happens when the tools used to fight one of the deadliest cancers fail to tell the full story, and how can a new approach change the game? Glioblastoma, an aggressive brain cancer with a survival rate of less than 15 months for most patients, has long evaded effective treatment, but a groundbreaking method involving serial biopsies is uncovering hidden battles within tumors that standard imaging misses. This innovative technique, paired with an engineered virus therapy known as CAN-3110, offers a glimpse into a tumor’s real-time response, challenging decades-old practices. Could this be the turning point in a fight that has seen little progress?
The significance of this development cannot be overstated. Glioblastoma claims thousands of lives each year, with current therapies often falling short due to an incomplete understanding of how tumors evolve under treatment. Serial biopsies, as demonstrated in recent research by a collaborative team of experts, provide a detailed, molecular-level view of these changes, revealing immune responses invisible to MRI scans. This story explores how such a method could redefine treatment strategies, offering hope to patients facing a grim prognosis and potentially altering the trajectory of brain cancer care.
A Fresh Perspective on a Lethal Cancer
Traditional approaches to glioblastoma have relied heavily on surgery, radiation, and chemotherapy, yet outcomes remain dismal. Most patients face recurrence within months, and the tools used to monitor progress—primarily MRI scans—often paint an incomplete picture. These scans can suggest tumor growth when, in reality, something more complex is unfolding beneath the surface. The inability to capture these nuances has left clinicians with limited options, often guessing at the effectiveness of a given therapy.
Enter serial biopsies, a technique that involves taking multiple tissue samples from a tumor over time. This method, though invasive, allows researchers to observe the dynamic shifts within the tumor microenvironment with unprecedented clarity. Unlike imaging, which focuses on visible changes, biopsies reveal cellular and molecular transformations that signal whether a treatment is sparking an immune response or failing to make an impact. This distinction is critical for a disease as aggressive as glioblastoma.
The potential of this approach lies in its ability to challenge long-held assumptions. For years, a growing tumor on a scan was seen as a definitive sign of treatment failure. Now, evidence suggests that what appears as progression might actually be the immune system mobilizing against the cancer. This shift in perspective could redefine how success is measured, moving the field toward more accurate and personalized interventions.
The Flaws in Current Glioblastoma Strategies
Despite advances in medical technology, glioblastoma treatment remains stuck in a frustrating cycle of trial and error. Standard protocols often involve aggressive interventions that yield limited results, with many patients surviving less than a year post-diagnosis. The reliance on MRI scans to track tumor growth or shrinkage has proven inadequate, as these images fail to reflect the deeper biological changes occurring within the cancer itself.
This gap in understanding has significant consequences. Without real-time data on how a tumor responds at a cellular level, clinicians struggle to adjust therapies mid-course. A treatment might be abandoned prematurely if a scan suggests failure, even if unseen mechanisms are at work. The need for a more precise tool has become increasingly urgent as innovative therapies, such as oncolytic virus treatments, demand a better way to gauge their impact.
Serial biopsies address this critical blind spot by offering a direct look into the tumor’s evolving landscape. By repeatedly sampling tissue during treatment, researchers can track shifts that imaging cannot detect, such as the replacement of cancer cells with immune fighters. This method promises to bridge the divide between what is seen and what is truly happening, paving the way for more informed clinical decisions.
Peering into Tumors with Serial Biopsies
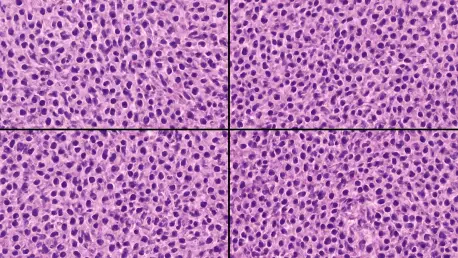
Recent studies have showcased the power of serial biopsies through a small but revealing trial involving two glioblastoma patients treated with CAN-3110, an engineered virus therapy. Over four months, multiple tissue samples were collected, allowing researchers to map changes in the tumor microenvironment with striking detail. What emerged was a picture far different from what MRI scans suggested.
Key findings included a notable decrease in tumor cell content near the virus injection sites, replaced by activated immune cells like CD8+ and CD4+ T cells. These cells appeared to target both the virus and glioblastoma-specific markers, a response that standard imaging misrepresented as disease progression. Through advanced techniques such as single-cell RNA sequencing and AI-driven pathology, the team uncovered a hidden immune battle that could signal the therapy’s effectiveness.
This approach not only challenges conventional metrics but also highlights the limitations of relying solely on visual data. The ability to analyze tumors at a molecular level offers a clearer understanding of treatment dynamics, suggesting that what looks like failure might be a critical step toward success. Such insights are invaluable for refining therapies and ensuring patients receive the most effective care possible.
Expert Insights Driving Change
Prominent voices in cancer research are championing the shift toward serial biopsies as a game-changing tool. Dr. E. Antonio Chiocca, a leading neurosurgeon at Brigham and Women’s Hospital, describes the technique as a “real-time window” into tumor behavior, urging the field to move beyond an over-reliance on imaging. His perspective reflects a growing consensus that deeper data is essential for tackling glioblastoma’s complexity.
Dr. Tyler Jacks, President of Break Through Cancer, emphasizes the collaborative effort behind this research, involving top institutions like Dana-Farber Cancer Institute and MIT’s Koch Institute. He views this teamwork as a model for accelerating innovation, noting that early trial results show serial biopsies are tolerable for patients, with no major adverse effects reported in the initial cohort. This finding is crucial for scaling the approach to larger studies.
These expert opinions underscore a pivotal moment in brain cancer research. By prioritizing molecular evidence over visual cues, the medical community can redefine what constitutes progress in treatment. The preliminary data from this trial fuels optimism that serial biopsies could become a cornerstone of future protocols, provided ongoing research continues to validate their safety and impact.
Crafting a New Path for Glioblastoma Care
The implications of serial biopsies extend far beyond a single study, offering a potential blueprint for transforming glioblastoma treatment. Integrating this method into clinical trials could provide detailed data on how therapies like CAN-3110 perform, starting with small groups to ensure safety and refine techniques. Such steps are vital for building confidence in this invasive yet insightful approach.
Another key focus is redefining how progression is interpreted. Medical teams must be trained to analyze radiographic data alongside cellular findings, avoiding hasty conclusions about a treatment’s failure. Additionally, leveraging advanced analytics—such as multi-omics and AI tools—can help identify patterns in biopsy data, predicting which patients might benefit most from specific interventions. This precision is a cornerstone of personalized medicine.
Ultimately, the goal is to adapt treatment plans in real time based on a tumor’s evolving response. By tailoring therapies mid-course, clinicians can maximize effectiveness and improve quality of life for patients facing this devastating diagnosis. This adaptive strategy marks a departure from the rigid, one-size-fits-all methods of the past, pointing toward a future where glioblastoma care is as dynamic as the disease itself.
Reflecting on a Bold Step Forward
Looking back, the journey to integrate serial biopsies into glioblastoma treatment marked a daring shift in perspective. Researchers and clinicians alike grappled with the limitations of traditional imaging, recognizing that true progress demanded a deeper dive into the tumor’s inner workings. The early trials with CAN-3110 therapy stood as a testament to the power of persistence, revealing immune responses that scans alone could not capture.
As the field moved forward, the focus shifted to actionable next steps. Expanding the use of serial biopsies in larger clinical studies became a priority, alongside efforts to educate medical professionals on interpreting molecular data. The collaboration among leading institutions served as a reminder that innovation thrives on shared expertise, setting a precedent for tackling other complex cancers.
Beyond these immediate goals, the broader vision was to empower patients with treatments tailored to their unique biology. Continued investment in advanced analytics and interdisciplinary research promised to refine this approach, ensuring that glioblastoma care evolved with each new discovery. This path, though challenging, offered a renewed sense of possibility for those affected by a once-intractable disease.