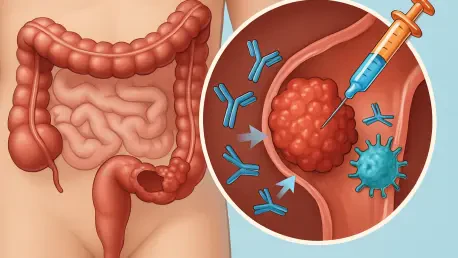
Imagine a scenario where a patient diagnosed with metastatic colorectal cancer (CRC) receives a treatment that not only halts the disease’s progression but also leads to remarkable tumor shrinkage, offering a renewed chance at life. This isn’t just a hopeful vision but a reality for a small subset of patients, thanks to groundbreaking research uncovering the role of specific genetic mutations in predicting immunotherapy success. A recent study from a leading cancer research center has shed light on how rare mutations in the POLE gene can dramatically influence treatment outcomes for CRC patients. This discovery is poised to transform the approach to personalized medicine, ensuring that therapies are tailored to those most likely to benefit. By identifying which patients will respond exceptionally well to immune checkpoint therapy, the findings pave the way for more effective and targeted interventions in a disease that remains one of the leading causes of cancer-related deaths worldwide. This advancement underscores the critical need to delve deeper into genetic profiling as a cornerstone of modern oncology.
Unraveling the Role of POLE Mutations in Immunotherapy
Recent research has honed in on the POLE gene, revealing that not all mutations within this gene carry the same weight when it comes to predicting responses to immunotherapy in colorectal cancer patients. The study distinguishes between different types of POLE mutations, identifying a rare subset known as loss-of-proofreading (LOP) mutations that are strongly linked to exceptional treatment outcomes. Unlike other mutations in the same gene, LOP variants impair specific protein functions, resulting in a heightened response to immune checkpoint therapy. This finding is significant because it explains why some patients experience dramatic tumor reduction while others, despite having POLE mutations, see little to no benefit. The differentiation between mutation types marks a pivotal shift in understanding immunotherapy’s variable efficacy, emphasizing that genetic nuances matter greatly in clinical settings. Such insights are driving a more refined approach to identifying candidates for specific therapies, ensuring that treatment plans are as precise as possible.
Building on this discovery, the data paints a striking picture of the potential held by LOP mutations. In a detailed analysis of thousands of cancer patients, POLE mutations were found to occur in just 2.8% of tumors across various cancer types, with LOP variants being even rarer at a mere 0.1%. However, among a smaller clinical group of CRC patients with these specific mutations, the results were nothing short of extraordinary. An impressive 88.9% overall response rate and a complete 100% disease control rate were observed when treated with immunotherapy. This stark contrast with patients carrying non-LOP mutations highlights a critical disparity in treatment outcomes based on genetic profiles. The rarity of these mutations does not diminish their importance; instead, it underscores the urgent need for advanced genetic testing to pinpoint those who stand to gain the most from cutting-edge therapies. This research is a testament to the power of precision in tackling complex diseases like CRC.
Personalizing Treatment Through Genetic Insights
The implications of identifying LOP POLE mutations extend far beyond academic interest, directly impacting how treatment decisions are made for colorectal cancer patients. Tumor sequencing has emerged as an indispensable tool in this context, enabling clinicians to determine the exact type of mutation a patient carries before initiating therapy. For those with LOP mutations, immunotherapy offers a promising path with significantly better outcomes compared to standard treatments. Conversely, for patients with non-LOP variants, alternative approaches can be explored to avoid ineffective therapies that might delay more suitable interventions. This tailored strategy aligns with the broader movement in oncology toward personalized medicine, where treatments are customized based on individual genetic markers. Such precision not only enhances the likelihood of success but also minimizes unnecessary side effects, improving the overall quality of care for those battling metastatic CRC.
Further exploration of this research reveals its potential to reshape clinical practices on a larger scale. By integrating detailed genetic analysis into routine diagnostics, healthcare providers can better stratify patients into groups based on their likelihood of responding to specific treatments. This approach eliminates much of the guesswork traditionally associated with cancer therapy, replacing it with data-driven decisions. For the small but significant subset of CRC patients with LOP mutations, this could mean access to life-changing immunotherapy with unprecedented success rates. Meanwhile, the focus on genetic profiling encourages the development of new tools and technologies to detect these rare mutations more efficiently. As the field of oncology continues to evolve, the emphasis on such personalized strategies will likely become a standard, ensuring that every patient receives the most effective care possible based on their unique biological makeup. This shift represents a profound step forward in the fight against colorectal cancer.
Charting the Future of CRC Care
Reflecting on the strides made through this research, it’s clear that the identification of LOP POLE mutations as predictors of immunotherapy success marks a turning point in colorectal cancer management. The remarkable response rates observed in patients with these rare mutations provide a beacon of hope for improved outcomes through targeted therapies. Looking ahead, the focus should shift toward expanding access to genetic testing, ensuring that more patients can benefit from precise mutation classification. Developing standardized protocols for tumor sequencing could streamline the process, making it a routine part of diagnosis and treatment planning. Additionally, future clinical trials should prioritize incorporating genetic profiling to refine therapy selection further. Collaboration among researchers, clinicians, and technology developers will be essential to overcome the challenges posed by the rarity of these mutations, ultimately paving the way for innovative solutions that enhance personalized care in oncology.