In a world where medical advancements have conquered countless diseases, a silent yet deadly threat looms large—drug-resistant fungal infections are claiming millions of lives each year, often with little public attention. These infections strike hardest at the most vulnerable, such as cancer patients, organ transplant recipients, and those battling severe illnesses that weaken immune defenses. Current antifungal treatments frequently fall short against resistant strains, leaving healthcare providers grappling with limited options. The urgency for innovative solutions has reached a critical point, as the global death toll from fungal infections surpasses 3 million annually. Amid this crisis, a groundbreaking collaboration between the Hackensack Meridian Center for Discovery and Innovation (CDI) and the Johns Hopkins Bloomberg School of Public Health offers a beacon of hope. Announced in November, this partnership, supported by substantial federal funding, aims to revolutionize the fight against these lethal pathogens through cutting-edge research and development.
Unveiling a Growing Health Crisis
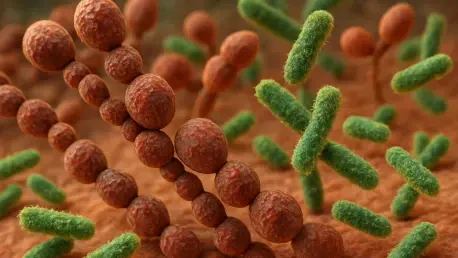
The scale of the challenge posed by drug-resistant fungal infections cannot be overstated, as they have quietly evolved into a major public health emergency. Strains like Candida auris, flagged by the CDC as an “urgent antimicrobial resistance threat,” alongside Candida glabrata and Aspergillus fumigatus, often resist even the strongest antifungal drugs available today. This resistance creates a formidable barrier for medical professionals, especially when treating immunocompromised patients who are at heightened risk of fatal outcomes. The statistics paint a grim picture—millions of deaths occur globally each year due to invasive fungal infections, a number that continues to climb as resistance spreads. Unlike bacterial or viral threats, fungal pathogens have historically received less focus in medical research, despite their devastating impact. This lack of attention has allowed the problem to fester, making the need for targeted interventions all the more pressing in modern healthcare systems.
Beyond the raw numbers, the human cost of these infections reveals a deeper tragedy that demands immediate action from the scientific community. Patients undergoing life-saving treatments like chemotherapy or organ transplants often find themselves defenseless against fungal invaders that exploit their weakened states. Hospitals, meant to be places of healing, can become breeding grounds for resistant strains like Candida auris, which spreads rapidly in clinical settings. The frustration among clinicians is palpable as they watch existing medications fail, leaving them with few tools to save lives. Public health experts have begun sounding the alarm, describing fungal resistance as an “existential threat” that could rival other antimicrobial resistance crises if left unchecked. Addressing this issue requires not just awareness but a concerted push for innovation, as traditional approaches to treatment are no longer sufficient against such adaptable and deadly organisms.
Harnessing Collaboration for Breakthroughs
The fight against drug-resistant fungal infections has gained a powerful ally through the newly established Center of Excellence in Translational Research (CETR), a collaborative effort led by the Hackensack Meridian CDI and Johns Hopkins Bloomberg School of Public Health. This initiative unites a diverse consortium, including academic powerhouses like Rutgers University and industry leaders such as Prokaryotics, Scynexis, and Cepheid Diagnostics, to pool expertise and resources. Backed by the National Institute of Allergy and Infectious Diseases (NIAID), the CETR receives approximately $7 million annually for a projected five years, subject to funding availability. This significant financial support underscores the federal commitment to tackling a crisis that threatens global health security. By blending academic rigor with practical industry know-how, the partnership is poised to drive meaningful progress in a field desperate for new solutions.
What makes this collaboration stand out is its emphasis on creating a seamless pipeline from research to real-world application, ensuring that scientific discoveries don’t remain theoretical. The involvement of biopharma and diagnostic companies means that innovations can be tested, refined, and scaled for clinical use at an accelerated pace. Leaders like Dr. David Perlin from CDI and Dr. Arturo Casadevall from Johns Hopkins bring decades of expertise in fungal infections and microbiology, guiding the initiative with strategic vision. A Scientific Advisory Board, composed of prominent figures in antimicrobial research, further strengthens the effort by providing oversight and direction. This multidisciplinary model serves as a blueprint for how complex health challenges can be addressed through teamwork, offering a framework that could inspire similar efforts in other areas of medicine facing resistance crises.
Driving Innovation Through Tangible Outcomes
At the heart of the CETR’s mission lies a commitment to translational research, a process that transforms laboratory findings into practical tools for patient care. The center has set ambitious goals to deliver a comprehensive portfolio to the FDA, including two small-molecule drug candidates ready for Investigational New Drug (IND) status, a pioneering immunotherapy, and a point-of-care diagnostic for bloodstream infections poised for 510(k) clearance. These deliverables are not mere aspirations but concrete targets designed to address the glaring gaps in current treatment options for drug-resistant fungi. By focusing on both therapeutic and diagnostic advancements, the initiative aims to equip healthcare providers with a robust arsenal to combat infections that have long evaded effective management, ultimately saving countless lives.
This push for innovation aligns closely with the broader movement toward precision medicine, a paradigm that prioritizes tailored interventions over one-size-fits-all approaches. The development of rapid diagnostic tools under the CETR framework promises to revolutionize how fungal infections are identified, allowing for quicker, more accurate detection at the bedside. Meanwhile, targeted therapies, such as the proposed immunotherapy, could offer new hope for patients who fail to respond to conventional drugs. These advancements hold the potential to improve outcomes significantly by ensuring that treatments are matched to specific pathogens and patient profiles. As resistant fungi continue to challenge global health systems, such forward-thinking strategies are essential to staying ahead of evolving threats and mitigating the devastating toll of these infections on vulnerable populations.
Charting the Path Forward
Reflecting on the strides made, the establishment of the CETR marked a pivotal moment in the battle against drug-resistant fungal infections, bringing together top-tier institutions and industry experts under a unified mission. The substantial backing from NIAID provided a critical foundation for this work, enabling a focus on developing new drugs, immunotherapies, and diagnostics that addressed a crisis claiming millions of lives annually. The collaborative spirit, guided by seasoned leaders and a dedicated advisory board, set a high standard for what could be achieved through shared purpose and expertise. Challenges, such as the complexity of fungal resistance and funding uncertainties, were acknowledged, yet the initiative’s comprehensive approach offered a strong basis for optimism.
Looking ahead, the next steps involve sustaining momentum by ensuring that research translates into accessible clinical tools as swiftly as possible. Stakeholders must prioritize streamlining regulatory pathways to bring these innovations to market, while also investing in global surveillance to track resistant strains. Partnerships like this one should inspire further funding and collaboration across other neglected areas of antimicrobial resistance. Ultimately, the lessons learned from this effort could pave the way for a more resilient healthcare landscape, better equipped to handle emerging threats and protect the most vulnerable from the silent scourge of fungal infections.