A groundbreaking analysis presented at the European Association of Cardiovascular Imaging 2025 congress has shed new light on a critical and burgeoning field of medicine, revealing that treating valvular heart disease in cancer patients can dramatically improve their survival rates. As remarkable advancements in oncology extend the lives of millions, a new frontier of patient care has emerged, focused on managing the long-term health complications that arise in cancer survivors. Among the most pressing of these is cardiovascular disease, which can be both a pre-existing condition and a direct consequence of life-saving cancer therapies. The comprehensive CESAR study addresses this intersection head-on, providing compelling evidence that a proactive, targeted approach to managing heart valve conditions in this vulnerable population is not merely beneficial but is an essential component of comprehensive cancer care that can significantly alter patient outcomes.
The Intersection of Cancer and Heart Health
A Growing Concern The Cardiotoxic Effects of Cancer Therapy
The link between a cancer diagnosis and subsequent cardiovascular complications is a well-recognized clinical challenge, stemming from a dual-pronged risk. Firstly, as cancer survivors live longer, they naturally enter an age demographic where the incidence of cardiac issues, including valvular heart disease (VHD), rises. Secondly, and more directly, many cornerstone cancer treatments are known to possess cardiotoxic properties. Potent therapies such as certain types of chemotherapy and radiation, while effective at eradicating cancer cells, can inflict collateral damage on the heart muscle and its delicate valve structures. This can either precipitate the onset of VHD or accelerate the progression of a pre-existing condition. Dr. Maximilian Autherith of the Medical University of Vienna, the study’s presenter, specifically noted that anthracycline chemotherapy is a known agent capable of inducing heart failure, which can then lead to secondary regurgitation, or leakage, in the tricuspid and mitral valves. Despite this established connection, a significant void in clinical evidence has persisted, leaving physicians with little definitive guidance on the optimal management strategy for VHD in cancer patients. This uncertainty has created a pervasive question of whether these complex patients derive the same survival benefits from valvular interventions as individuals without a history of cancer, often leading to a more conservative, and potentially detrimental, treatment approach.
This long-standing uncertainty in clinical practice formed the impetus for a deeper investigation into the cardiovascular health of cancer patients. The lack of robust, large-scale data meant that decisions regarding heart valve interventions were often made on a case-by-case basis, heavily influenced by a physician’s individual experience and a perceived high risk of surgical or procedural complications in the oncology population. This has fostered a climate of what some experts term “therapeutic nihilism,” where potentially life-saving cardiac procedures may be withheld due to the presence of a cancer diagnosis, regardless of its stage or prognosis. Clinicians have been caught in a difficult position, weighing the immediate risks of an intervention against the poorly quantified long-term benefits for a patient already burdened with a serious illness. The critical need was for evidence that could clarify the true prevalence of severe VHD in this group, its actual impact on mortality independent of the cancer itself, and, most importantly, whether the benefits of intervention outweigh the risks. Without such data, the standard of care remained ambiguous, and a significant opportunity to improve long-term survival for a growing population of cancer survivors was potentially being missed. The CESAR study was designed specifically to fill this void and provide the clarity needed to build new, evidence-based clinical guidelines.
The CESAR Study Seeking Answers
To address this critical knowledge gap, investigators designed and conducted the CESAR (Concomitant Valvular Heart Disease in Cancer Patients) study, a large-scale, observational cohort analysis with three primary objectives. The first goal was to accurately determine the prevalence of VHD among patients with a confirmed cancer diagnosis. Secondly, the study aimed to document the frequency with which these patients underwent corrective interventions for their valve disease, whether through traditional surgery or less invasive transcatheter procedures. The third and most crucial objective was to rigorously evaluate the impact of these interventions on patient survival, thereby answering the central question of their efficacy in this specific population. The research team meticulously analyzed a vast dataset comprising 10,353 adult patients who not only had a confirmed cancer diagnosis but had also undergone a transthoracic echocardiogram at a single tertiary referral center over a 12-month period. This methodology ensured a focused and consistent cohort for analysis, allowing for a detailed examination of the relationship between cancer, heart valve function, and long-term outcomes in a real-world clinical setting.
The demographic profile of the patient cohort was carefully documented to ensure the findings were relevant and generalizable to the broader population facing these concurrent diagnoses. The mean age of the 10,353 patients was 66.2 years, an age where both cancer and degenerative heart disease become more prevalent. The gender distribution was nearly even, with 46.6% of the participants being female, reflecting the broad impact of these health issues across both sexes. By including a large number of patients with diverse cancer types and a range of cardiovascular risk factors, the study was well-positioned to draw powerful and statistically significant conclusions. The use of transthoracic echocardiography as a baseline inclusion criterion provided a standardized, non-invasive method for assessing cardiac structure and function across the entire cohort. This rigorous study design, encompassing a substantial and well-characterized patient group, provided a solid foundation for producing the high-quality evidence needed to inform future clinical practice and reshape the burgeoning field of cardio-oncology.
Uncovering the Stark Reality of VHD in Cancer Patients
Alarming Prevalence and Deadly Consequences
The results of the CESAR study were both illuminating and deeply concerning, revealing that severe valvular heart disease is a far more common comorbidity in cancer patients than previously understood. Within the large cohort, a significant 7.2% of patients were found to have at least one form of severe VHD. The most frequently observed condition was severe tricuspid regurgitation, a condition where the valve between the two right heart chambers fails to close properly, affecting 3.7% of the study population. This was followed by severe mitral regurgitation, a similar leakage problem on the left side of the heart, which was present in 2.6% of patients. Finally, severe aortic stenosis, a dangerous narrowing of the valve controlling blood flow out of the heart, was identified in 2.2% of individuals. These figures collectively demonstrate that severe, hemodynamically significant valvular disease is not a rare occurrence but a substantial clinical issue affecting a notable portion of cancer patients referred for cardiac imaging. The findings immediately shift the perception of VHD from an occasional complication to a common and serious co-existing condition that warrants systematic attention.
Beyond simply establishing a high prevalence, the research powerfully demonstrated that the presence of severe VHD was a formidable and independent predictor of mortality. After performing a rigorous statistical analysis that adjusted for other influential factors—including patient age, sex, kidney function, left ventricular function, and levels of key cardiac biomarkers—the link between severe VHD and poor outcomes remained remarkably strong. The data confirmed that severe VHD independently increased the risk of all-cause mortality by a significant 46% (adjusted Hazard Ratio [HR] 1.46; 95% Confidence Interval [CI] 1.25-1.71). The impact on death specifically due to cardiovascular causes was even more profound and alarming. Severe VHD was associated with a staggering 162% increased risk of cardiovascular-specific death (adjusted HR 2.62; 95% CI 2.00-3.43). This data unequivocally proves that severe VHD is not a benign or secondary finding in the context of cancer but is, in fact, a major independent driver of adverse outcomes and a direct threat to patient survival, separate from the prognosis of their underlying malignancy.
A Tale of Two Outcomes The Treatment Gap and Its Impact
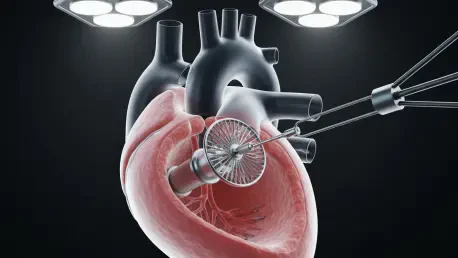
Despite the clear and present danger posed by severe VHD, the study uncovered a significant and troubling gap in patient care. Among the sizable group of patients identified with severe and life-threatening valvular conditions, only a small fraction—just 21.5%—received a definitive therapeutic intervention to correct the problem. These interventions could have taken the form of traditional open-heart surgery to repair or replace the valve or, increasingly, a less invasive transcatheter approach where a new valve is delivered via a catheter. This low rate of intervention suggests a widespread tendency toward a conservative, non-interventional approach for cancer patients, likely rooted in concerns about the perceived risks of such procedures in a medically complex population. This finding highlights a critical area for improvement in clinical practice, as a large majority of patients with a deadly yet treatable heart condition were not receiving the therapy that could potentially extend their lives. The data points to a systemic underutilization of effective cardiac treatments within the oncology setting, revealing a major unmet need for this vulnerable patient group.
In stark contrast to the low treatment rates, the outcomes for the minority of patients who did undergo a valvular intervention were extraordinary. This finding represents the most impactful message of the entire study: treating severe VHD in cancer patients yields a profound survival benefit. The analysis demonstrated that receiving a valvular intervention was independently associated with a remarkable 72% reduction in mortality risk compared to not receiving an intervention (adjusted HR 0.28; 95% CI 0.09-0.87) over a median follow-up period of 23 months. This dramatic improvement in survival powerfully refutes the notion that such interventions are futile or overly risky in the context of a cancer diagnosis. It underscores the profound efficacy of treating the heart valve disease directly, suggesting that the cardiovascular condition is a major contributor to mortality that can be successfully mitigated. The immense survival benefit observed in the treated group provides a compelling, evidence-based argument against therapeutic nihilism and advocates for a more aggressive and proactive approach to managing severe VHD in cancer patients.
Charting a New Course for Cardio-Oncology
The comprehensive findings from the CESAR study decisively established that severe valvular heart disease was a common and highly lethal comorbidity in cancer patients, yet the life-saving interventions designed to correct it appeared to be significantly underutilized. The results strongly suggested that a prevailing conservative approach, perhaps driven by an overestimation of procedural risks in this population, was ultimately detrimental to patient survival. These conclusions carried significant implications for the rapidly evolving field of cardio-oncology, highlighting an urgent need for the implementation of systematic cardiovascular monitoring and screening programs. Such programs would be particularly crucial for patients undergoing potentially cardiotoxic cancer treatments. Furthermore, the powerful survival benefit associated with intervention served as a compelling argument against withholding valvular treatments from patients based on their oncology diagnosis alone. The research advocated for a proactive, interdisciplinary strategy where oncologists and cardiologists collaborate closely to optimize the care and long-term health of their shared patients. The next phase of this research was set to involve a more granular analysis, aimed at differentiating outcomes based on specific cancer therapies and intervention types, which would further refine clinical guidelines for this complex and growing patient population.