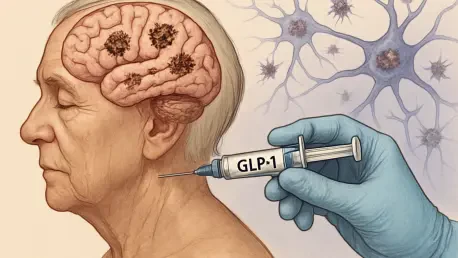
In a world where Alzheimer’s disease continues to challenge medical science with its relentless progression and devastating impact on millions of lives, the search for effective treatments remains a top priority for researchers and pharmaceutical companies alike. Recent developments have sparked curiosity about whether drugs initially designed for other conditions, such as GLP-1 receptor agonists like semaglutide, could offer a new frontier in battling this neurodegenerative disorder. Originally developed to manage diabetes and obesity, these medications have shown promise in early studies for their potential to address brain inflammation and improve neurological functions. However, the journey from hypothesis to proven therapy is fraught with obstacles, as demonstrated by the latest clinical trials. This article delves into the outcomes of significant studies conducted by a leading pharmaceutical company, exploring the implications of their findings, the broader challenges in Alzheimer’s research, and what the future might hold for GLP-1 drugs in this complex field.
Unveiling the Trial Results
The recent completion of two large-scale clinical trials, known as Evoke and Evoke+, has brought critical insights into the potential of semaglutide for treating early-stage Alzheimer’s disease. These studies, involving over 3,800 participants, were designed to assess whether this GLP-1 drug could preserve brain function and slow the progression of the disease over a two-year period. Disappointingly, the results indicated that semaglutide did not outperform a placebo in achieving these primary goals. Despite this setback, there were subtle signs of improvement in certain biological markers associated with Alzheimer’s, though specific data remains undisclosed at this stage. Due to the underwhelming outcomes, the decision was made to halt the one-year extension phases of both trials. Detailed findings are anticipated to be shared at upcoming medical conferences in the coming months, offering a deeper understanding of where semaglutide stands in this context and whether there are any silver linings to be explored further in subsequent analyses.
Beyond the headline results, the trial outcomes shed light on the intricate nature of applying a drug like semaglutide, primarily known for metabolic benefits, to a neurological condition as multifaceted as Alzheimer’s. Early research had fueled optimism by suggesting that GLP-1 drugs could combat brain inflammation, reduce harmful protein accumulation, and enhance insulin signaling, which plays a vital role in memory and mood regulation. However, the failure to meet primary endpoints echoes previous disappointments with similar drugs in the same class, such as liraglutide, which also showed minor cognitive benefits but fell short of significant impact in mid-stage trials. This pattern underscores the daunting reality that translating theoretical benefits into measurable clinical success remains elusive. The commitment to continued exploration, despite low expectations of immediate breakthroughs, reflects the urgent unmet need for effective Alzheimer’s therapies and the willingness to push boundaries in drug development.
Industry Perspectives and Competitive Dynamics
Analysts and industry experts have long viewed Alzheimer’s as an exceptionally tough target for drug developers, a sentiment reinforced by the recent trial results of semaglutide. Market expectations for these studies were notably low, with financial analysts expressing skepticism about the likelihood of transformative outcomes. This cautious outlook stems from the historical difficulty in achieving meaningful progress against Alzheimer’s, even with drugs showing promise in other therapeutic areas. Interestingly, the failure of semaglutide in this context may have a ripple effect across the pharmaceutical landscape. For companies already in the Alzheimer’s space, such as those marketing anti-amyloid treatments like Leqembi, this setback could reduce competitive pressure and potentially boost their market share. Conversely, a successful trial might have heightened disease awareness and paved the way for innovative combination therapies, blending GLP-1 drugs with existing treatments to tackle multiple disease pathways simultaneously.
Shifting focus to the broader pharmaceutical industry, particularly in the realm of obesity and incretin therapies, the impact of these trial results appears limited for other major players. Competitors are often pursuing neurological applications of incretin therapies in areas distinct from Alzheimer’s, such as substance use disorders, rather than focusing on neurodegenerative diseases. This diversification suggests that while the setback with semaglutide is notable, it does not broadly disrupt research trajectories in the incretin space. Financial markets reacted swiftly to the news, with a significant drop in share prices for the company behind semaglutide, highlighting the high stakes and investor sensitivity surrounding clinical trial outcomes in high-profile areas like Alzheimer’s. As the industry continues to evolve, there is an expectation that more neurology-focused trials will emerge, reflecting sustained interest in the potential of GLP-1 and related therapies to address a wide range of conditions beyond their original metabolic applications.
Exploring Future Pathways
Despite the disappointing trial outcomes, there remains a thread of cautious optimism about the role GLP-1 drugs like semaglutide could play in Alzheimer’s treatment through alternative strategies. Experts from leading research foundations have pointed out that the observed improvements in biological markers, though not fully detailed yet, might indicate potential when used in combination with other therapies. Current anti-amyloid drugs slow cognitive decline by only about 30%, leaving a significant gap that treatments targeting different mechanisms, such as GLP-1s, could help bridge. This perspective aligns with a growing consensus in the field that a multifaceted approach, integrating various therapeutic pathways, is essential to address the complexity of Alzheimer’s. The possibility of combining semaglutide with existing treatments opens up new avenues for research, emphasizing the need for innovative trial designs that test synergistic effects rather than standalone efficacy.
Looking ahead, the focus must shift toward sustained investment and creative problem-solving to overcome the persistent challenges in Alzheimer’s drug development. The industry’s response to these trial results reflects a broader recognition that setbacks are part of the journey toward breakthroughs in such a difficult area. Financial and scientific resources should be directed toward exploring combination therapies and identifying patient subgroups that might benefit most from GLP-1 interventions. Additionally, leveraging advanced biomarker analysis and imaging technologies could provide deeper insights into how these drugs interact with Alzheimer’s pathology at a molecular level. As detailed trial data becomes available in the coming months, it will be crucial to analyze every aspect of the findings to inform future studies. Ultimately, the path forward lies in resilience and adaptability, ensuring that each disappointment serves as a stepping stone toward more effective solutions for those affected by this debilitating disease.