For countless families touched by Huntington’s disease (HD), a genetic neurodegenerative disorder with no cure or disease-modifying treatments, the struggle against an inevitable decline has been a heartbreaking reality, but a beacon of hope emerged on September 24, 2025. On that date, uniQure announced groundbreaking results for its gene therapy, AMT-130, revealing a striking 75% slowdown in disease progression over 36 months during clinical trials. This remarkable development could herald a new era in managing HD, a condition that relentlessly impairs movement, cognition, and emotional well-being. With existing treatments limited to symptom management, the potential of AMT-130 to alter the disease’s trajectory offers a profound shift in perspective. This article delves into the therapy’s unprecedented efficacy, the urgent needs it addresses, the challenges ahead, and the evolving landscape of HD care, exploring whether gene therapy can truly transform the fight against this devastating illness.
Breaking New Ground in Efficacy
The clinical results of uniQure’s AMT-130 mark a historic turning point in the battle against Huntington’s disease. Data from Phase I/II trials, specifically the HD-GENE-TRX1 and HD-GENE-TRX2 studies, demonstrated a statistically significant 75% reduction in disease progression over a 36-month period, as assessed by the composite Unified Huntington’s Disease Rating Scale. Compared to a propensity-matched external control group, patients receiving AMT-130 exhibited a slower decline, a finding that stands out in a field where no prior therapy has altered the disease’s course. This achievement is not merely a statistical success but a potential lifeline for those facing the progressive loss of motor and cognitive functions. The therapy’s ability to impact the underlying mechanisms of HD, rather than just masking symptoms like involuntary movements, positions it as a pioneering advancement that could redefine patient outcomes.
Beyond the headline figures, AMT-130 also met crucial secondary endpoints that underscore its transformative potential. Notably, the therapy significantly slowed the decline in total functional capacity, a key measure of a patient’s ability to perform daily activities independently. This outcome resonates deeply with the HD community, where maintaining independence is a paramount concern as the disease progresses. Unlike current treatments that focus narrowly on managing chorea or psychiatric symptoms, AMT-130 offers a glimpse of sustained quality of life. While the sample size for the high-dose group reaching the 36-month mark remains small, the consistency of these results fuels cautious optimism among researchers and clinicians. If sustained in larger studies, this efficacy could establish gene therapy as a cornerstone of HD management, shifting the narrative from mere survival to meaningful living.
Meeting a Long-Standing Unmet Need
Huntington’s disease has long been a therapeutic desert, with patients and families desperate for options beyond symptomatic relief. Key opinion leaders in the field have repeatedly highlighted the absence of disease-modifying treatments, a gap that AMT-130 is poised to fill as a potential first-in-class therapy. Supported by encouraging 36-month data, the treatment has garnered significant regulatory recognition, including orphan drug, fast-track, and regenerative medicine advanced therapy designations from the FDA. These statuses not only validate the therapy’s promise but also expedite its path to market, with a biologics license application slated for submission in the first quarter of 2026 and possible approval by the second half of that year. Such momentum suggests that a groundbreaking option could soon be within reach for those in dire need.
The impact of addressing this unmet need extends beyond clinical metrics to the emotional and societal burden of HD. Families affected by the disease often face a hereditary cycle of suffering, knowing that a genetic mutation places future generations at risk. AMT-130’s potential to slow progression offers not just a medical intervention but a psychological reprieve, alleviating some of the dread tied to an HD diagnosis. Industry experts have expressed optimism about the therapy’s role in transforming the standard of care, particularly as it targets the root genetic cause rather than peripheral symptoms. While challenges remain in ensuring broad access and acceptance, the prospect of a treatment that fundamentally alters the disease’s trajectory represents a monumental shift, potentially setting a precedent for how genetic disorders are managed in modern medicine.
Navigating Significant Challenges
Despite the excitement surrounding AMT-130, substantial barriers stand in the way of its widespread adoption. The exorbitant cost of gene therapies is a primary concern, often leading to reimbursement hurdles and restricted access for many patients. Given the specialized nature of such treatments, payers and healthcare systems may grapple with justifying the expense, particularly in regions with constrained budgets. This financial obstacle risks creating disparities, where only a fraction of those in need can benefit from this cutting-edge approach. Until pricing models or assistance programs evolve to bridge this gap, the therapy’s reach could be limited, leaving many HD patients reliant on less effective, symptomatic treatments despite the availability of a potentially life-changing option.
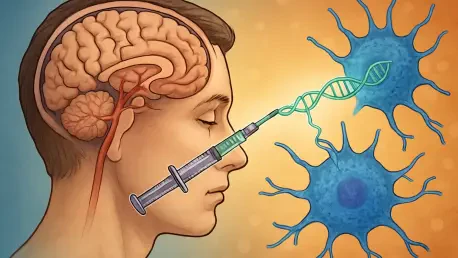
Equally daunting is the complex and invasive method required to administer AMT-130, which involves MRI-guided, convection-enhanced stereotactic neurosurgery. This procedure, while precise, may not be suitable for all patients due to medical ineligibility or personal reluctance to undergo such an intensive intervention. Furthermore, the logistical demands of delivering this treatment place a significant burden on healthcare infrastructure, requiring specialized facilities and trained personnel that may not be universally available. Safety considerations also linger, even though no serious adverse events have been reported since enhanced monitoring protocols were implemented following a temporary trial pause in 2022. The irreversible nature of gene therapy and the limited long-term data from small cohorts continue to prompt caution among experts, highlighting the need for rigorous post-approval surveillance to ensure patient safety over extended periods.
Exploring a Diverse Treatment Landscape
While AMT-130 stands as a frontrunner in HD treatment innovation, it is unlikely to serve as a universal solution for all patients. The broader competitive landscape reveals a dynamic field, with multiple companies pursuing alternative strategies to combat the disease. For instance, antisense oligonucleotides are being developed by entities like Roche and Wave Therapeutics, aiming to reduce the toxic huntingtin protein at the RNA level. Meanwhile, firms such as PTC Therapeutics, Novartis, and Skyhawk Therapeutics are focusing on oral drugs that target similar pathways with the added advantage of non-invasive administration. This variety underscores the recognition that no single therapy will address every patient’s needs, paving the way for a more inclusive approach to HD management that could complement gene therapy’s role.
The diversity in therapeutic development also reflects a growing consensus among experts that accessibility and patient preference are critical to treatment success. Oral medications, if proven effective, could bypass the logistical and psychological barriers associated with invasive procedures like those required for AMT-130. Such alternatives might democratize access to disease-modifying options, particularly for individuals in underserved regions or those wary of surgical interventions. Industry analysts project significant market growth over the coming years, with AMT-130 potentially achieving blockbuster status. However, the presence of competing modalities ensures that the HD treatment space remains open to innovation, fostering an environment where patients might eventually choose from a spectrum of options tailored to their unique circumstances and medical profiles.
Envisioning a Future of Tailored Solutions
The trajectory of HD care is undeniably shifting toward disease-modifying therapies, with AMT-130 leading as a beacon of progress in this transformation. Industry consensus points to a market ripe for innovation, driven by the stark absence of treatments that address the underlying genetic mechanisms of the disease. Gene therapy’s promising results signal a potential paradigm shift, establishing it as a viable strategy despite its inherent challenges. This movement aligns with a broader trend toward personalized medicine, where the focus is on crafting interventions that match the specific genetic and lifestyle profiles of patients, ensuring that therapeutic impact is maximized for each individual affected by HD.
Looking ahead, the emphasis on tailored solutions highlights the necessity of continued research and collaboration across the medical and pharmaceutical sectors. The success of AMT-130, while groundbreaking, serves as a stepping stone rather than a final answer, prompting further exploration into how diverse therapies can coexist to serve a heterogeneous patient population. Experts advocate for sustained investment in both invasive and non-invasive approaches, recognizing that patient choice and accessibility will shape the future of HD care. As regulatory pathways accelerate and clinical data accumulate, the next few years promise to reveal whether gene therapy can anchor a new standard of treatment, ultimately offering hope to thousands navigating the challenges of this relentless condition.