I’m thrilled to sit down with Ivan Kairatov, a renowned biopharma expert whose pioneering work in technology and innovation has pushed boundaries in medical research and development. With a deep focus on cutting-edge solutions, Ivan has been at the forefront of exploring focused ultrasound as a transformative approach to treating brain cancer in children. Today, we’ll dive into the challenges of pediatric brain cancer, the groundbreaking potential of this non-invasive technology, and the hope it brings for improving survival rates. Our conversation will touch on how this method tackles barriers in drug delivery, the outcomes of recent studies, and what the future might hold for young patients battling this devastating disease.
Can you explain what focused ultrasound is and how it helps in treating brain cancer in children?
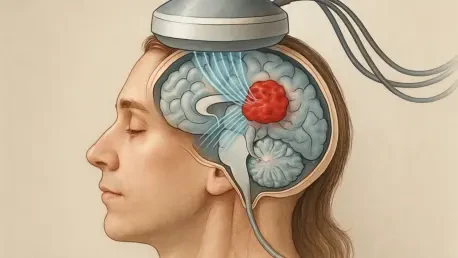
Focused ultrasound is a non-invasive technology that uses sound waves to target specific areas in the brain. It’s particularly exciting for treating brain cancer in kids because it helps overcome one of the biggest hurdles: getting drugs into the brain. The sound waves are directed at the blood-brain barrier, a protective shield around the brain, and they work with tiny lipid-coated gas bubbles that are injected into the bloodstream. When the sound waves hit these bubbles, they vibrate, expand, and contract, temporarily opening small pathways in the barrier. This allows chemotherapy drugs to pass through and reach the tumor in much higher concentrations than would otherwise be possible. It’s a game-changer for ensuring the medication gets where it’s needed most.
Why is treating brain cancer, especially diffuse midline glioma, such a significant challenge for doctors?
Brain cancer, and particularly diffuse midline glioma in children, is incredibly tough to treat due to its location and biology. This type of cancer starts deep in the brainstem, a critical area controlling vital functions like breathing and heart rate, which makes surgical options nearly impossible. On top of that, the blood-brain barrier acts as a fortress, blocking most chemotherapy drugs from reaching the tumor in effective doses. This barrier is essential for protecting the brain from toxins and infections, but it also severely limits treatment options. As a result, survival rates for kids with midline glioma are heartbreakingly low, often less than a year after diagnosis, compared to much better outcomes for other pediatric cancers. It’s a stark reminder of how much work is still needed in this field.
What inspired your team to explore focused ultrasound as a treatment option for children with brain cancer?
Our team saw focused ultrasound as a potential breakthrough because of its ability to address the blood-brain barrier issue without invasive procedures. We were driven by the dire need for new approaches in pediatric brain cancer, where traditional therapies have fallen short for decades. The technology had shown promise in lab studies and adult applications, so we wanted to adapt it for children, who often face unique vulnerabilities. We knew there were risks, especially in ensuring precision and safety with such young patients, but the potential to improve drug delivery and offer even a small chance of better outcomes was worth pursuing. It was about giving these kids and their families a fighting chance.
Can you share some insights from your study involving children with diffuse midline glioma and the impact of focused ultrasound?
In our initial study, we worked with a small group of children diagnosed with diffuse midline glioma, and the results were encouraging, even if bittersweet. Using focused ultrasound, we successfully opened the blood-brain barrier in all the patients, which allowed the chemotherapy to penetrate the brain and reach the tumors. We observed some improvement in mobility in the children, which was a meaningful sign that the treatment was having an effect on the tumor environment. Unfortunately, the long-term outcomes weren’t what we hoped for, as the disease and other complications took their toll. Still, these findings were a crucial first step, proving that the technique is feasible and safe in children, and it gave us invaluable data to build on for future trials.
I understand your approach involved performing the procedure outside an MRI machine, which is unconventional. Why was this significant for the children?
Moving the focused ultrasound treatment outside the MRI machine was a big deal for the comfort and well-being of the kids. Typically, these procedures require patients to lie still in an MRI for guidance, which can be incredibly stressful, especially for children who may already be anxious or unwell. Our team developed a hand-guided device using pre-obtained MRI images for planning, so the actual treatment could happen in a more relaxed setting. The kids could rest on a comfortable table, play on a tablet, or read a book, with their families nearby. It’s a brief, painless process lasting just a few minutes, and making it less intimidating was a priority for us. It’s about reducing trauma wherever we can in their treatment journey.
What are the next steps for focused ultrasound in treating pediatric brain cancer following your initial findings?
We’re already moving forward with a follow-up trial that pairs focused ultrasound with a chemotherapy drug called etoposide, which has shown promise against brain cancer cells. The goal is to refine the approach and test whether higher drug concentrations in the brain can make a bigger impact. We’re also exploring the possibility of using this technology earlier in the disease process, when tumors might be more responsive, and potentially combining it with other medications. Each trial builds on the last, helping us understand how to optimize timing, dosing, and safety. It’s a slow but deliberate process, and every piece of data brings us closer to a viable treatment strategy for these children.
How do you envision focused ultrasound shaping the future of brain cancer treatment for kids?
I believe focused ultrasound has the potential to revolutionize how we treat brain cancer in children by fundamentally changing how we deliver therapies. If we can consistently and safely open the blood-brain barrier, we could unlock the full potential of existing drugs that are already effective against cancer cells but currently can’t reach the brain in sufficient amounts. Beyond that, it opens doors to developing new drugs specifically designed to work with this technology. I see a future where this approach could be part of standard care, used early in diagnosis to improve survival rates and quality of life. It’s not a cure on its own yet, but it’s a powerful tool that could transform the landscape of pediatric oncology in the coming decades.
What is your forecast for the future of focused ultrasound in pediatric brain cancer treatment?
My forecast is cautiously optimistic. Over the next five to ten years, I expect we’ll see significant advancements in how focused ultrasound is integrated into treatment protocols, especially as we gather more data from ongoing trials. With improvements in device precision and a better understanding of which drugs pair best with this method, we could start seeing meaningful extensions in survival for kids with brain cancers like diffuse midline glioma. I also anticipate broader applications, potentially for other neurological conditions in children. The key will be collaboration across engineering, oncology, and regulatory fields to ensure the technology is accessible and safe. It’s a challenging road, but I truly believe this could become a cornerstone of hope for families facing these devastating diagnoses.