I’m thrilled to sit down with Ivan Kairatov, a renowned biopharma expert whose extensive experience in research and development has positioned him at the forefront of innovation in cancer treatment. With a deep understanding of cutting-edge technologies, Ivan has been exploring groundbreaking strategies to tackle some of the toughest challenges in oncology. Today, we’ll dive into his insights on cancer stem cells (CSCs) and a promising new approach to target them through ferroptosis, a unique form of cell death. Our conversation will touch on the challenges posed by CSCs, the science behind ferroptosis, and how this strategy could revolutionize cancer therapy by addressing treatment resistance and recurrence.
Can you start by explaining what cancer stem cells are and why they’re such a significant hurdle in cancer treatment?
Cancer stem cells, or CSCs, are a small subset of cells within a tumor that have the ability to self-renew and differentiate into various cell types that make up the tumor. Think of them as the root of the cancer—they can regenerate the tumor even after treatment. What makes them such a big challenge is their resistance to conventional therapies like chemotherapy and radiation. Unlike regular cancer cells, CSCs often remain dormant and have mechanisms to protect themselves from oxidative stress, making them incredibly hard to kill. This resilience is why many treatments fail to prevent cancer from coming back.
How does ferroptosis stand out as a form of cell death compared to more familiar processes like apoptosis or necrosis?
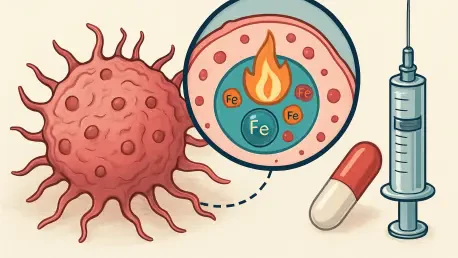
Ferroptosis is quite distinct because it’s driven by iron-dependent lipid peroxidation, which is essentially the breakdown of lipids in cell membranes due to oxidative damage. Unlike apoptosis, which is a programmed and orderly cell death, or necrosis, which is more chaotic and inflammatory, ferroptosis hinges on the accumulation of toxic lipid peroxides triggered by iron. This process disrupts the cell’s protective mechanisms, like glutathione levels, leading to catastrophic damage. It’s a fascinating pathway because it offers a new way to target cells that evade other death mechanisms.
What makes cancer stem cells particularly susceptible to ferroptosis compared to other cancer cells?
CSCs have a unique iron metabolism that sets them apart. They tend to take up more iron than non-stem cancer cells, which is likely a survival mechanism to support their growth and resilience. However, this high iron level also makes them vulnerable to ferroptosis, as the excess iron can catalyze the production of damaging reactive oxygen species, or ROS, through lipid peroxidation. Additionally, CSCs often maintain low ROS levels to protect themselves, but ferroptosis-inducing strategies can overwhelm this defense, tipping the balance toward cell death. It’s like exploiting their own strength against them.
Could you walk us through some of the innovative approaches being developed to trigger ferroptosis in these resistant cells?
Absolutely. One promising strategy involves inhibiting SLC7A11, a transporter protein that brings cysteine into cells to produce glutathione, a key antioxidant. By blocking SLC7A11, we reduce glutathione levels, making CSCs more susceptible to oxidative damage from lipid peroxidation. Another exciting avenue is the use of nanoparticle drug delivery systems. These can be designed to increase intracellular iron and ROS specifically in CSCs, enhancing the ferroptosis effect while minimizing damage to healthy cells. These targeted approaches are showing a lot of potential in preclinical studies.
How could targeting ferroptosis in CSCs help address the issue of cancer recurrence or resistance to existing therapies?
Cancer recurrence often happens because CSCs survive initial treatments and later regenerate the tumor. By targeting ferroptosis, we’re hitting these root cells directly, reducing the likelihood of the cancer coming back. Additionally, since CSCs are a major driver of therapy resistance, inducing ferroptosis can make existing treatments like chemotherapy more effective by eliminating the cells that would otherwise persist. It’s a complementary strategy that could enhance the overall impact of cancer therapy, potentially leading to longer-lasting remissions.
What are some of the challenges or uncertainties that still need to be addressed when using ferroptosis as a treatment strategy?
One major challenge is ensuring selectivity. While CSCs are more vulnerable to ferroptosis due to their iron metabolism, there’s still a risk of affecting healthy cells, especially those with high iron levels like in the liver or heart. We need to fine-tune these therapies to target only cancer cells. Another uncertainty is the long-term effects and optimal dosing of ferroptosis-inducing agents. There’s also a lot we don’t fully understand about the interplay between ferroptosis and other cellular processes in the tumor environment. More research is crucial to address these gaps and ensure safety.
What is your forecast for the future of ferroptosis-based therapies in cancer treatment?
I’m very optimistic about the potential of ferroptosis-based therapies. In the next decade, I believe we’ll see significant progress in developing targeted drugs and delivery systems that can precisely induce ferroptosis in CSCs without harming healthy tissues. As our understanding of CSC biology and ferroptosis mechanisms deepens, I expect these therapies to become a key component of personalized cancer treatment, especially for patients with resistant or recurrent cancers. It’s an exciting field, and with continued research and collaboration, I think we’re on the cusp of a major breakthrough.