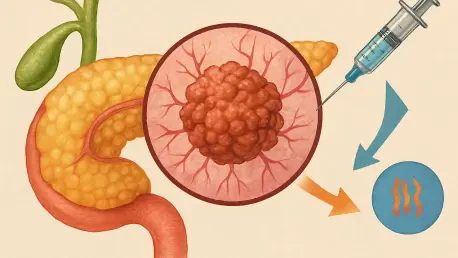
Pancreatic cancer stands as one of the most formidable adversaries in the realm of oncology, with survival rates often tragically limited to mere months after diagnosis, highlighting the urgent need for innovative solutions. The relentless nature of this disease, coupled with its resistance to conventional treatments like chemotherapy and radiation, underscores the critical demand for new approaches. A recent study conducted by researchers at The Institute of Cancer Research (ICR) in London has sparked hope with a pioneering approach that combines two experimental therapies. Published in the esteemed journal Pharmaceutics and backed by Pancreatic Cancer UK, this research introduces a dual therapy strategy that could potentially alter the landscape of treatment. By targeting the tumor’s protective barriers and boosting immune responses, this method offers a fresh perspective on tackling a cancer notorious for its dismal prognosis. This article explores the intricacies of this groundbreaking approach, delving into its mechanisms, challenges, and the path forward for transforming patient outcomes.
Unpacking the Dual Therapy Approach
Harnessing Ultrasound with Boiling Histotripsy
Boiling histotripsy represents a cutting-edge, non-invasive technique that utilizes focused ultrasound pulses to mechanically disrupt tumor tissue in a highly targeted manner. Within just a few hours, this method induces visible cellular damage, breaking down the physical structure of pancreatic tumors without the need for invasive surgery. The study demonstrated that histotripsy effectively reduces the presence of regulatory T cells, which are known to dampen immune responses and protect tumors from attack. By diminishing these suppressive cells, the treatment creates a more conducive environment for the body’s natural defenses to engage with the cancer. Notably, the research was conducted using orthotopic mouse models, where tumors are positioned in the pancreas to closely mimic human conditions, ensuring that the findings are as relevant as possible to real-world applications. This precision-driven approach highlights the potential of histotripsy as a game-changer in minimizing patient discomfort while maximizing therapeutic impact.
Beyond its immediate physical effects, boiling histotripsy offers a strategic advantage by altering the tumor microenvironment in ways that conventional treatments often fail to achieve. The mechanical disruption not only damages cancer cells directly but also exposes hidden tumor components to the immune system, potentially triggering a broader anti-cancer response. This aspect of the therapy is particularly significant for pancreatic cancer, where the dense, protective stroma surrounding tumors often shields them from immune detection. By breaking through these barriers, histotripsy sets the stage for complementary treatments to amplify their effectiveness. The use of orthotopic models in the study further validated these effects under conditions that replicate the complex anatomical challenges faced in human patients. As a standalone method or part of a combined strategy, this ultrasound-based technique could redefine how aggressive tumors are approached, paving the way for less invasive yet highly potent interventions.
Activating Immunity Through Oncolytic Reovirus Therapy
Oncolytic reovirus therapy introduces a biological weapon into the fight against pancreatic cancer by employing viruses engineered to selectively infect and destroy cancer cells. This innovative treatment goes beyond mere destruction, as it simultaneously stimulates the immune system to recognize and attack the tumor more effectively. The research revealed that this therapy significantly reduces macrophages, a type of cell that often suppresses immune activity within the tumor microenvironment, thus weakening the cancer’s defenses. When paired with other treatments, the reovirus approach showed a marked increase in immune activation, demonstrating its potential as a synergistic tool. The realistic setting of orthotopic mouse models ensured that these immune dynamics were observed in a context mirroring human pancreatic cancer, providing valuable insights into how this therapy might translate to clinical success.
The broader implications of oncolytic reovirus therapy lie in its ability to transform the immune landscape surrounding pancreatic tumors, a critical factor in overcoming treatment resistance. By selectively targeting cancer cells while leaving healthy tissue unharmed, this viral strategy minimizes collateral damage and focuses the body’s defenses where they are most needed. The reduction in immune-suppressing macrophages observed in the study points to a shift in the tumor’s protective mechanisms, making it more vulnerable to attack. Furthermore, the immune stimulation triggered by the reovirus can potentially lead to long-term benefits, as the body learns to recognize and combat cancer cells more efficiently. Tested in a biologically accurate model, these findings underscore the therapy’s promise as part of a multi-faceted approach, offering a glimpse into a future where immunotherapy plays a central role in managing one of the deadliest cancers known to medicine.
Navigating Obstacles and Future Horizons
Confronting the Neutrophil Challenge
A significant finding from the study was the unexpected role of neutrophils, a type of white blood cell typically associated with fighting infections, in hindering the effectiveness of the dual therapy. In the context of pancreatic tumors, these cells were found to emit signals that not only weaken immune responses but also promote tumor growth, countering the benefits of the treatment. Surprisingly, the combination of boiling histotripsy and oncolytic reovirus therapy appeared to attract more neutrophils to the tumor site, exacerbating this detrimental effect. This discovery marks a departure from prior research, which often emphasized other immune cells like macrophages as primary barriers to treatment. The complex interplay between neutrophils and the tumor microenvironment reveals just how intricate cancer biology can be, posing a critical challenge that must be addressed to fully realize the potential of this innovative therapeutic strategy.
Addressing the neutrophil issue requires a deeper understanding of their behavior within pancreatic tumors and how they interact with both the cancer and the immune system. The study’s findings suggest that simply enhancing immune responses may not suffice if certain cell types counteract these efforts. This nuanced perspective shifts the focus toward developing targeted interventions that can neutralize or redirect neutrophils without compromising other beneficial immune activities. The research team’s use of advanced analytical techniques to map immune cell populations and gene expression provided critical data on these dynamics, laying the groundwork for future innovations. As a pivotal obstacle, the role of neutrophils underscores the need for a more comprehensive approach to cancer therapy, one that accounts for the full spectrum of immune interactions rather than targeting isolated components of the disease.
Charting the Path Forward with Enhanced Strategies
To tackle the counterproductive effects of neutrophils, the research team has proposed a three-part treatment framework that integrates a component to block or modulate neutrophil activity alongside boiling histotripsy and oncolytic reovirus therapy. This refined strategy aims to preserve the immune-boosting and tumor-disrupting benefits of the dual approach while mitigating the negative impact of these white blood cells. Led by Dr. Petros Mouratidis and Professor Gail ter Haar, the team remains committed to advancing this concept through additional preclinical studies, with the ultimate goal of slowing tumor progression and improving survival rates. Such a multi-pronged method could set a new standard for personalized cancer care, not just for pancreatic cancer but potentially for other resistant solid tumors as well.
Looking ahead, the journey from preclinical research to clinical application will require meticulous testing and validation to ensure safety and efficacy in human patients. The proposed three-part strategy represents a forward-thinking solution that balances innovation with practicality, acknowledging the complexity of tumor biology. Beyond neutralizing neutrophils, future research may explore additional immune modulators or complementary therapies to further enhance treatment outcomes. The insights gained from orthotopic models provide a solid foundation for these next steps, offering a realistic preview of how such interventions might perform in real-world scenarios. As this field evolves, the commitment to addressing every facet of the tumor microenvironment will be crucial in transforming experimental therapies into tangible hope for those battling one of the most lethal forms of cancer.