The COVID-19 pandemic has brought unprecedented challenges to global health, but recent research suggests it may also offer unexpected benefits. Scientists from the Northwestern Medicine Canning Thoracic Institute have discovered a surprising link between the immune response to COVID-19 and cancer regression. This groundbreaking study, published in The Journal of Clinical Investigation, explores how the body’s reaction to the SARS-CoV-2 virus could pave the way for innovative cancer treatments.
The Unexpected Discovery
Inducible Nonclassical Monocytes (I-NCMs)
Researchers found that RNA from the SARS-CoV-2 virus induces the formation of a unique type of immune cell known as inducible nonclassical monocytes (I-NCMs). These cells exhibit remarkable anti-cancer properties, offering a new perspective on cancer treatment. Unlike typical immune cells, I-NCMs have specific receptors that allow them to infiltrate tumor environments and attack cancer cells directly. This specific ability to penetrate and operate within tumor cells distinguishes I-NCMs from other immune cells, underlining their potential significance in fighting cancer.
The research revealed that these newly formed I-NCMs do more than just enter the cancer battlefield. Once within these tumor environments, they initiate an immune response that involves the release of certain chemicals attracting natural killer cells. These natural killer cells then work to identify and destroy cancer cells. The process suggests that a component of our immune response to COVID-19 could potentially be harnessed to fight cancer, making the connection between the virus’s RNA and these uniquely capable cells an exciting development.
Mechanism of Action
The study took a deeper look into the mechanism of how the RNA from SARS-CoV-2 leads to the transformation of regular monocytes into I-NCMs. It was found that the RNA activates specific immune signals that fundamentally alter the behavior of these white blood cells. Unlike their typical function of patrolling blood vessels, these I-NCMs are triggered to possess specific receptors that allow them to enter tumor sites. There, they emit necessary chemicals that summon natural killer cells to the scene.
The arrival of these natural killer cells marks the beginning of an assault on the cancer cells. The immune signals activated by the RNA guide the transformation of monocytes into I-NCMs, which in turn recruit natural killer cells to the tumor site. This cascade of immune reactions stands out as a novel method by which the body’s defense systems can be mobilized against cancer cells, suggesting that viral RNA might be a hidden ally in cancer therapy.
Potential Therapeutic Applications
Preclinical Effectiveness
In preclinical animal models, researchers demonstrated that I-NCMs could be pharmacologically stimulated using small molecules. This approach showed effectiveness against various cancers, including melanoma, lung, breast, and colon cancer. The ability to induce these unique immune cells pharmacologically opens up new therapeutic options for patients with advanced or aggressive cancers. Importantly, this discovery provides a fresh insight into cancer treatment modalities, which have primarily relied on conventional methods up until now.
The preclinical results indicated that these immune cells could be activated in a controlled manner through pharmacological agents. This could mean significant advancements for patients whose cancers have not responded to traditional treatments, offering hope where options have previously been limited. The success of these preclinical trials is an encouraging step toward potential new therapies that target these I-NCMs specifically, presenting a shift in how we might approach cancer therapy in the future.
Clinical Potential
While the findings are promising, extensive clinical trials are necessary to determine the safety and effectiveness of this approach in human patients. If successful, this method could provide a transformative solution for treating cancers that have exhausted existing treatment modalities. The potential to develop therapies targeting I-NCMs specifically could revolutionize cancer treatment by expanding the arsenal of tools available to oncologists, especially in treating more resistant forms of cancer.
The researchers are keenly aware that translating these findings from preclinical models to human patients involves substantial testing and validation. These clinical trials will be crucial in understanding how best to harness I-NCMs’ properties for therapeutic use and assessing any potential side effects or risks. Despite the early stage of this research, the premise carries significant promise for future cancer treatments, signifying a potentially groundbreaking shift in medical science.
Implications for Existing Cancer Programs
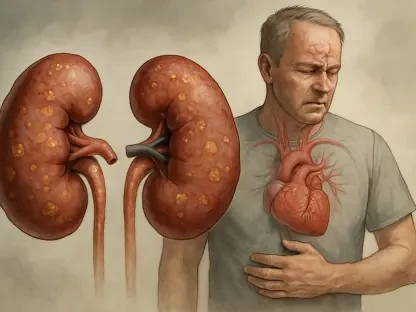
Integration with DREAM Program
The research has significant implications for Northwestern Medicine’s Double Lung Replacement and Multidisciplinary Care (DREAM) Program. This program treats patients with advanced lung cancers through double-lung transplants. By incorporating the findings on I-NCMs, there may be a way to treat cancer recurrences in DREAM patients without risking lung transplant rejection. This integration reflects a highly innovative application of the recent research findings and could profoundly impact patient care protocols.
The challenge of treating cancer recurrences in transplant patients is particularly acute, given the delicate balance required to avoid transplant rejection. The introduction of I-NCMs could offer a new strategy by employing the body’s own immune system to manage and minimize the risk of returning cancer cells. Incorporating these findings into the DREAM program could increase the success rates of lung transplants and improve overall patient outcomes, thereby setting a new standard in cancer treatment protocols.
Broader Impact on Cancer Treatment
The connection between COVID-19’s immune response and cancer regression underscores the potential of immunotherapy in cancer treatment. This discovery aligns with the growing interest in leveraging the body’s immune system to fight cancer, a fundamental principle behind current immunotherapies. The innovative application of these findings could lead to new treatment protocols and improved outcomes for cancer patients. The concept of harnessing an immune response triggered by a virus to combat cancer represents a novel frontier in medical research.
This broader impact could revolutionize how cancer is treated on multiple levels, prompting a reevaluation of existing treatment methodologies and the development of novel therapeutic approaches. Furthermore, it places immunotherapy at the forefront of cancer research, reinforcing the trend of using the body’s natural defenses as a key line of attack against tumors. This connection offers a fresh perspective on how diseases can be intertwined in ways that may yield unexpected benefits, fostering a deeper understanding of the immune system’s role in health and disease management.
Future Directions and Research
Need for Clinical Trials
The researchers emphasize the necessity for extensive clinical trials to validate their findings. These trials will help ascertain the safety and effectiveness of using I-NCMs in cancer treatment. Successful trials could lead to the development of new therapies that harness the body’s immune response to combat cancer. The rigorous process of clinical validation is essential to ensure the safe application of these promising findings to real-world medical practice, ensuring that therapies are both effective and without considerable adverse effects.
The buildup to human trials must navigate through phases of testing, each designed to evaluate different aspects of safety, dosage, and overall efficacy. These efforts are made to establish whether the therapeutic benefits observed in preclinical models will safely translate to human patients. The researchers’ commitment to a meticulous trial process reflects the importance of thoroughly vetted treatments in the quest to offer innovative and reliable options for cancer therapy.
Potential for Broader Applications
The ongoing study of the immune response to COVID-19 has unearthed a surprising connection to cancer regression. Researchers at the Northwestern Medicine Canning Thoracic Institute have shown that certain immune responses triggered by the SARS-CoV-2 virus may also target cancer cells. This discovery offers hope for novel cancer therapies that harness the body’s natural ability to fight off viral infections.
Despite the challenges posed by the COVID-19 pandemic, this research highlights the potential for unforeseen breakthroughs in cancer treatment. By leveraging the immune system’s defense mechanisms against viruses, scientists may develop innovative therapies that transform how cancer is managed. The findings hold the promise of advancing cancer treatment, providing new hope for patients and paving the way for groundbreaking medical advancements.