The medical landscape has been witnessing a groundbreaking shift with the advent of novel therapies aimed at tackling some of the most challenging conditions. One such development is the Phase 1/2 clinical trial of Cabaletta Bio’s CAR T-cell therapy, rese-cel (resecabtagene autoleucel), targeting adults with hard-to-treat systemic sclerosis (SSc), also known as scleroderma. The trial, RESET-SSc (NCT06328777), is currently recruiting participants across various sites in the U.S. and focuses on individuals aged 18-75 who have severe skin, heart, lung, and/or kidney involvement. This innovative approach offers hope to many who have struggled with the debilitating effects of this condition.
The Mechanism of CAR T-Cell Therapy
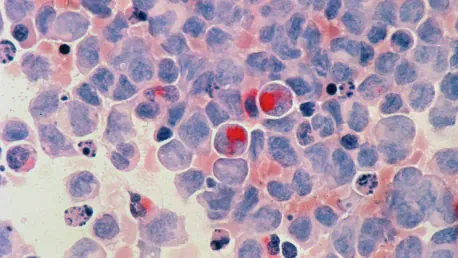
Scleroderma is a perplexing disease characterized by inflammation and fibrosis, leading to the accumulation of scar tissue in the skin and internal organs. Central to its pathology are hyperactive B-cells that produce antibodies, which damage healthy tissues. The novel CAR T-cell therapy aims to address this by modifying a patient’s T-cells to express a chimeric antigen receptor (CAR) that targets CD19, a protein found on B-cells. Once these altered T-cells are reinfused, they seek out and deplete the B-cells, thereby reducing inflammation and fibrosis.
Early results from the RESET-SSc study have shown promising clinical improvements. Specifically, there have been significant advancements in skin condition and lung function three months post-infusion in the first patient with severe skin involvement. This patient had ceased all disease-specific therapies, indicating the potential transformative effects of the treatment. Such promising results have garnered strong interest from both physicians and patients, as highlighted by Cabaletta’s CEO, Steven Nichtberger.
Preliminary Findings and Incidents
While the initial results are optimistic, the trial has not been without its challenges. A patient who was dosed despite having a fever, contrary to the protocol, developed immune effector cell-associated neurotoxicity syndrome (ICANS). Fortunately, the neurotoxicity was temporary and resolved with corticosteroids. Following a thorough review, the trial was permitted to continue with stricter pre-infusion protocols to ensure patient safety. This incident underscores the importance of meticulous adherence to protocols in clinical trials to safeguard patient well-being.
The RESET trial’s primary objective is to assess safety by monitoring side effects within 28 days of infusion. Secondary outcomes include evaluating changes in vital signs and pharmacological properties over a span of three years, alongside efficacy measured by the Combined Response Index in Diffuse Cutaneous Systemic Sclerosis (CRISS) criteria. The commitment to these rigorous evaluations is crucial as it ensures that the therapy is both effective and safe for wider clinical use.
Long-term Goals and Future Directions
The long-term goals of the RESET trial extend beyond preliminary safety and efficacy. Early results from the first ten patients across various autoimmune diseases have demonstrated promising safety and efficacy profiles, including significant B-cell depletion. Additional data from the trial has been eagerly anticipated, providing further insights into the therapy’s potential.
It is noteworthy that the FDA granted orphan drug designation to rese-cel, aiming to expedite its development for rare diseases affecting fewer than 200,000 people in the U.S. This designation speaks volumes about the critical need for innovative treatments in managing rare and complex conditions like systemic sclerosis. The structured protocol adjustments and continuous monitoring within the trial are essential to ensure the therapy’s success and broader applicability.
A Glimmer of Hope
The medical field is experiencing a transformative shift with the emergence of new therapies addressing some of the most challenging diseases. A notable advancement is Cabaletta Bio’s CAR T-cell therapy, known as rese-cel (resecabtagene autoleucel), currently in a Phase 1/2 clinical trial targeting adults with difficult-to-treat systemic sclerosis (SSc), also called scleroderma. The trial, named RESET-SSc (NCT06328777), is actively recruiting participants across various U.S. locations. It focuses on individuals aged 18-75 who suffer from severe involvement of the skin, heart, lungs, and/or kidneys. This groundbreaking approach brings hope to those who have been grappling with the debilitating impact of this condition. By targeting the underlying mechanisms of SSc, rese-cel aims to improve the quality of life for patients who have limited treatment options. The success of this trial could mark a significant milestone in the fight against systemic sclerosis and pave the way for more advanced treatments in the future.