Mental healthcare has long relied on subjective methods for diagnosing and treating conditions. The Diagnostic and Statistical Manual of Mental Disorders (DSM) has been the cornerstone of this approach, guiding clinicians through a polythetic diagnostic process based on observed symptoms and patients’ reports. However, this method often leads to imprecise treatments and varied patient outcomes. The advent of precision psychiatry, a data-driven approach leveraging biological measures known as biomarkers, promises to revolutionize mental healthcare by offering more accurate and personalized treatments.
The Limitations of Traditional Diagnostic Methods
The DSM and Its Challenges
For over a century, mental health professionals have used the DSM to diagnose and treat mental health conditions. This manual requires clinicians to determine if patients meet specific criteria for given disorders based on observed symptoms and patients’ reports. The polythetic nature of the DSM allows for a wide heterogeneity of patients with the same diagnosis. For example, a depression diagnosis can result from 200 different constellations of symptoms. This approach leads to varied and often imprecise treatments, complicating the management of mental health conditions.
The DSM’s reliance on subjective observations and patient-reported symptoms means that two patients diagnosed with the same condition might exhibit vastly different symptoms. For example, two individuals diagnosed with depression might only share one symptom, such as difficulty concentrating. Consequently, they could receive entirely different treatments, some of which may not be effective for their specific needs. This variability contributes to the trial-and-error nature of current mental health treatment strategies, often leading to poor patient outcomes and frustration among patients and clinicians alike.
The Impact on Patient Outcomes
The subjective nature of DSM-based diagnoses often results in treatments that are not tailored to individual patients, further complicating the effectiveness of mental healthcare. Two patients diagnosed with depression might share only one symptom, leading to different treatment responses, which can be ineffective or even detrimental. This variability can result in poor patient outcomes and a prolonged trial-and-error approach to finding effective treatments. Patients may face prolonged periods of suffering as they cycle through different treatments that may not address their unique needs.
Additionally, the lack of precise, personalized treatment options can stigmatize mental health conditions, as patients may feel misunderstood or marginalized within the healthcare system. The imprecision of traditional methods underscores the need for a more data-driven approach that can deliver accurate diagnoses and personalized treatments. This gap between diagnosis and effective treatment highlights the importance of innovation in mental healthcare, paving the way for precision psychiatry to make a significant impact.
The Promise of Precision Psychiatry
Introduction to Precision Psychiatry
Precision psychiatry aims to personalize mental healthcare by using data-driven methods to deliver effective and tolerable treatments faster than traditional approaches. The driving force behind this innovative method is the study and use of biological measures or biomarkers to identify and differentiate subtypes of psychiatric conditions. Researchers have investigated various biomarkers, including memory, genes, cognitive performance, speech, hormones, and gut microbes, to categorize patients into homogeneous “biotypes.”
By incorporating these biomarkers, precision psychiatry seeks to overcome the limitations of the DSM’s subjective diagnostic criteria. Instead of relying solely on observable symptoms and patient reports, precision psychiatry leverages data to provide more accurate and personalized treatments. This approach promises to reduce the trial-and-error nature of traditional treatment methods, offering patients quicker and more effective relief from their conditions.
The Role of Biomarkers
Biomarkers have shown compelling associations with mental health conditions, but their adoption in clinical trials has been limited. Using biomarkers to categorize patients can lead to more targeted and effective treatment decisions. One promising method for neurotyping involves measuring event-related potentials (ERPs), which are functional brain measurements collected through task-related brain activity evident in the electroencephalogram (EEG).
ERPs have been studied extensively and have shown high test-retest reliability and interpretability across various mental health conditions. Specific ERPs are associated with subtypes of depression and can predict the course of depression and outcomes of particular treatments. Researchers have used ERPs to study cognitive domains such as memory, attention, vision, and emotion, offering valuable insights into the complexities of mental health conditions. These biomarkers can differentiate subtypes of psychiatric conditions, providing a clearer understanding of the underlying mechanisms driving each patient’s symptoms.
Event-Related Potentials (ERPs) in Mental Health
Understanding ERPs
For decades, ERPs have been a focus of research in mental health due to their high test-retest reliability and interpretability. Studied since the 1960s, ERPs are functional brain measurements collected through task-related brain activity using an electroencephalogram (EEG). Certain ERPs are associated with specific subtypes of depression and can predict the course of depression and outcomes of particular treatments. Researchers have utilized ERPs to study various cognitive domains, including memory, attention, vision, and emotion.
ERPs provide a window into brain function and can reveal the neural basis of psychiatric conditions. These measurements can be taken non-invasively, making them well-suited for both research and clinical applications. By analyzing ERPs, researchers can gain insights into the neural mechanisms underpinning mental health conditions, enabling more precise and effective treatments. This approach stands in stark contrast to the subjective assessments of traditional diagnostic methods, offering a more objective and reliable pathway to understanding and treating mental health conditions.
ERPs and Depression
Promising ERP biomarkers for depression have focused on brain responses to rewards, emotional content, decision-making, and attention. These ERPs have not only been linked to depression but also accurately predicted individuals’ risk for depression and its development over time. For instance, a 2023 study of adolescents with depression found that an ERP associated with the response to emotional stimuli predicted responses to cognitive behavioral therapy. This finding underscores the potential of using ERPs as neural biomarkers for predicting treatment outcomes in adolescent depression.
By identifying ERP patterns associated with depression, clinicians can tailor treatments to address specific neural mechanisms. This targeted approach can improve the effectiveness of interventions and reduce the time it takes for patients to experience relief from their symptoms. The predictive power of ERPs offers a promising avenue for early intervention, potentially preventing the onset of severe depression in at-risk individuals. This proactive approach to mental healthcare represents a significant advancement over traditional methods, which often involve reactive treatments after symptoms have already become pronounced.
The Broader Implications of ERPs
ERPs in Anxiety and Other Conditions
Beyond depression, ERPs have shown promise in identifying and understanding other mental health conditions, such as anxiety disorders. A 2019 meta-analysis published in the Annual Review of Clinical Psychology concluded that ERPs could help identify psychopathology and chart the potential development of conditions from childhood. For example, the error-related negativity (ERN) ERP component has been instrumental in understanding the development of anxiety disorders and guiding treatment opportunities. This ERP reflects individuals’ response to making errors and has been linked to anxiety and obsessive-compulsive disorder (OCD).
A review in the International Journal of Psychophysiology further explored ERPs associated with emotion regulation, highlighting their relevance in mental health research. The study demonstrated that ERPs linked to rewards were closely tied to depression and could predict remission. Combining insights from various ERP components can enhance the precision of mental health diagnoses and treatments, leading to more effective interventions for a wide range of conditions.
Combining ERPs for Better Precision
Combining emotion- and reward-related ERPs offers a powerful tool for differentiating subtypes of depression and improving treatment precision. This approach can lead to more accurate diagnoses and highly personalized treatment plans, significantly enhancing the targeting and effectiveness of mental health treatments. By integrating multiple ERP components, clinicians can develop a comprehensive understanding of each patient’s neural profile, tailoring interventions to address their unique needs.
This multifaceted approach to mental healthcare can revolutionize the field, moving beyond the limitations of traditional diagnostic methods. Precision psychiatry’s emphasis on data-driven, personalized treatments aligns with broader trends in medicine, prioritizing patient-centered care. The integration of ERPs into clinical practice represents a significant step toward achieving this vision, offering hope for more effective and timely interventions for individuals struggling with mental health conditions.
Practical Applications and Future Directions
ERPs in Clinical Trials
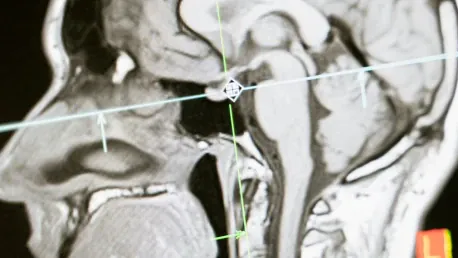
ERPs measured through EEG have demonstrated their value in scientifically valid research, both basic and applied. Incorporating ERPs into clinical trials offers a practical pathway for developing more personalized treatments. This approach can provide pharmaceutical companies with valuable insights into the neural mechanisms underlying psychiatric conditions, guiding the development of targeted interventions. However, psychiatry has traditionally leaned towards functional magnetic resonance imaging (fMRI) to measure brain activity.
While fMRI-based imaging studies are useful, they are expensive and often cost-prohibitive for clinical trials or routine tracking of mental health. Additionally, fMRI requires specialized training and equipment, making it challenging to scale this technology for widespread use. These limitations highlight the need for more accessible and cost-effective methods, such as EEG and ERPs, to advance precision psychiatry.
Advantages of EEG Over MRI
Capturing ERP data through EEG is more manageable and less expensive compared to MRI. Technological advancements have simplified the administration of EEG studies, which do not require as much training and expertise as MRI machines. Modern electrodes typically eliminate the need for conductive gels, making the process more tolerable and user-friendly for patients. Moreover, ERP measures of brain function have proven more reliable and reproducible than fMRI-based measures, enhancing their utility in clinical settings.
The economic and practical benefits of EEG and ERPs make them attractive options for expanding precision psychiatry. Their reliability, speed, and scalability can streamline clinical trials, enabling the development of new, personalized therapies with greater efficiency. By incorporating ERPs throughout the trial process, from participant recruitment to tracking brain function, pharmaceutical companies can ensure homogeneity among cohorts and support more rigorous and effective clinical research. This shift toward using ERPs in clinical practice promises to enhance the precision and impact of mental health treatments, offering new hope for patients and clinicians alike.
The Road Ahead for Precision Psychiatry
Technological Advancements
For a long time, mental healthcare has depended largely on subjective techniques to diagnose and treat disorders. Clinicians have mainly relied on the Diagnostic and Statistical Manual of Mental Disorders (DSM), a key resource that utilizes a polythetic diagnostic approach. This method is based on observed symptoms and patient reports, helping doctors make diagnoses by identifying patterns of symptoms. However, this traditional approach can often result in inaccurate treatments and inconsistent patient outcomes because it lacks objective measures.
Enter precision psychiatry, an innovative, data-driven method that has the potential to transform mental healthcare. Precision psychiatry employs biological markers, or biomarkers, to provide a more objective basis for diagnosis. These biomarkers can help pinpoint the specific underlying mechanisms of mental health conditions, allowing for tailored treatments that are more effective for individual patients.
By leveraging these biological measures, precision psychiatry aims to deliver more accurate diagnoses and personalized treatment plans, ultimately improving patient outcomes. This approach stands to resolve many issues inherent in the current polythetic method by offering clear, measurable criteria for diagnosis and treatment. As a result, the mental healthcare field is looking at a future where treatments are not only more precise but also more consistent, significantly enhancing patient care and recovery.