A recent international study is fundamentally changing the way clinicians understand and diagnose hereditary colorectal cancer, revealing that a direct analysis of colorectal polyp DNA can uncover critical information that standard blood tests frequently overlook. This groundbreaking research, a collaborative effort involving leading medical centers, offers a new pathway toward more precise diagnostics, personalized treatment strategies, and much-needed clarity for patients and their families who grapple with the uncertainty of genetic cancer risk. For a significant portion of individuals with a high number of polyps, a strong suspicion of hereditary predisposition has long been met with inconclusive genetic tests, leaving them and their relatives in a diagnostic limbo. This new approach, however, promises to resolve many of these complex cases by looking for genetic clues not in the blood, but within the very tissue where the potential for cancer begins, addressing a persistent and frustrating gap in modern oncology and paving the way for more effective preventative care.
The Diagnostic Dilemma of Unexplained Polyps
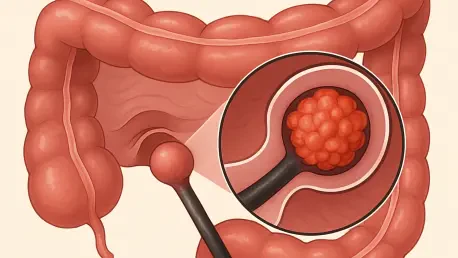
Colorectal cancer stands as one of the most prevalent cancers in the Western world, and it is well-established that hereditary factors play a role in approximately 5 to 10 percent of all diagnoses, with this percentage being notably higher among younger patients. A clinical suspicion of a genetic predisposition is typically triggered when an individual develops a large number of colorectal polyps, which are widely considered to be precursors to cancer. The established clinical guidelines for initiating a genetic investigation are quite specific, often recommending testing for individuals under 60 with at least 10 polyps or those under 70 with more than 20. While these patients routinely undergo genetic testing via DNA analysis of their blood, a definitive genetic cause is successfully identified in only about one-quarter of them. This frustratingly low success rate leaves the vast majority of these high-risk patients without a clear explanation for their condition, creating significant anxiety and complicating long-term health management for them and their families.
The diagnostic gap affecting the remaining 75 percent of these patients represents a significant challenge in oncology, leaving them in a state of prolonged uncertainty. For these individuals, the clinical evidence—a high burden of polyps at a relatively young age—strongly suggests an underlying hereditary risk, yet conventional genetic screening methods fail to provide an answer. This lack of a confirmed diagnosis has far-reaching consequences. Without a known genetic mutation, it becomes difficult to tailor surveillance protocols, such as the frequency of colonoscopies, to the patient’s specific risk level. Furthermore, genetic counseling for family members becomes incredibly complex, as it is impossible to determine which relatives may have inherited the same predisposition. This diagnostic void means that many families must navigate difficult decisions about preventative care and screening based on suspicion rather than concrete genetic evidence, a situation this new research sought to address directly by exploring an alternative source of genetic information.
A New Investigative Approach by Analyzing the Polyp Itself
To unravel the mystery surrounding this unresolved majority, a dedicated research team embarked on an extensive and innovative genetic analysis focused directly on the polyp tissue. The study was meticulously designed to include 180 individuals from across Europe who all fit a very specific and challenging clinical profile: they each presented with a high polyp burden but had no identifiable genetic cause found through traditional blood-derived DNA analysis. The core of this novel investigative strategy was the hypothesis that the genetic mutations responsible for the polyp growth might be confined to the colorectal tissue itself and therefore absent from the blood cells typically used for testing. By shifting the focus of the analysis from systemic DNA to the localized tissue, the researchers aimed to uncover genetic clues that could finally explain the development of these numerous growths and provide a definitive diagnosis where previous efforts had failed to do so. This targeted approach represented a logical next step in genetic diagnostics for this patient population.
The collaborative research, conducted within the framework of the Solve-RD consortium, involved a comprehensive examination of 333 polyps collected from the 180 study participants. This large-scale effort, uniting expertise from Radboud university medical center, university hospital Bonn, and partners in Munich and Barcelona, allowed for a robust and thorough investigation into the genetic underpinnings of these unexplained polyp cases. The team’s work went beyond simple gene sequencing; it involved a detailed analysis designed to detect subtle genetic abnormalities that might not be present in every cell of the body. By pooling resources and patient data from multiple European centers, the study achieved a level of statistical power and diversity that would be difficult to attain in a single-institution project. This international collaboration was instrumental in validating the findings across a broad patient population, ensuring that the results were not only scientifically significant but also clinically relevant for a diverse group of individuals facing the same diagnostic uncertainty.
Uncovering a Hidden Cause with the Mosaicism Breakthrough
The investigation yielded a clear and transformative set of findings, particularly for the 80 individuals in the study who had adenomatous polyps. While many of these growths were found to be caused by non-hereditary mutations in the well-known APC gene, the study revealed a far more significant underlying cause in a substantial portion of cases. In at least 20 percent of these individuals, the root of their condition was identified as a phenomenon known as APC mutational mosaicism. Mosaicism describes a complex genetic condition where a predisposition is not present in all of the body’s cells, as would be expected in a classic hereditary syndrome. Instead, the mutation is confined to a specific population of cells, such as those lining the large intestine. Because standard genetic tests rely on DNA extracted from blood cells, they are inherently unable to detect a mutation that is not present in the blood, thus providing a definitive explanation for why these patients’ previous tests had consistently returned negative results.
This landmark discovery not only identified the cause of polyp development in a significant subgroup but also provided crucial insights into the genetic landscape of these unexplained cases. The research strongly suggests that within the specific context of patients with numerous unexplained adenomatous polyps, the APC gene is likely the only gene where mosaicism plays a significant role. This finding helps to narrow the focus for future diagnostic efforts, indicating that when mosaicism is suspected in these patients, a targeted analysis of the APC gene in polyp tissue is the most effective and efficient strategy. By ruling out a broader range of mosaic mutations in other genes, the study provides a clearer diagnostic pathway and prevents a potentially lengthy and costly search for other genetic culprits. This specificity reinforces the importance of the APC gene in colorectal tumorigenesis and establishes a more direct route to diagnosis for a condition that has long puzzled clinicians and geneticists alike.
Redefining Family Risk and Patient Care
The identification of APC mosaicism has profound and immediate implications for patient care and the field of genetic counseling. It definitively establishes that for patients presenting with a high polyp burden and negative blood tests, a direct DNA analysis of the polyps is not just an option but a necessary next step to detect this hidden form of genetic predisposition. Receiving a diagnosis of mosaicism fundamentally alters the risk assessment for the patient’s family members, providing much-needed clarity. Unlike a traditional hereditary condition that is passed down through germline cells and present throughout the body, the risk profile for relatives of an individual with mosaicism is different. Crucially, the siblings of a person with APC mosaicism are not at an increased risk of developing the condition themselves. This is because the mutation occurred after fertilization and is not present in the parent’s reproductive cells, meaning it was not inherited and cannot be passed to siblings.
While siblings are not at elevated risk, the patient’s own offspring may still be at risk of inheriting the predisposition, making this information vital for family planning and determining future screening protocols. As lead researcher Stefan Aretz noted, this more comprehensive diagnostic work-up does more than just provide clarity to patients; it also relieves their relatives of unnecessary anxiety and can help exclude risk for the majority of their children. The ability to distinguish between mosaic and hereditary forms of the condition allows for more personalized and appropriate medical advice. It prevents relatives who are not at risk from undergoing unnecessary and invasive screenings, such as frequent colonoscopies, while ensuring that those who might be at risk—the patient’s children—receive the appropriate counseling and surveillance. This tailored approach represents a significant advance in precision medicine, focusing medical resources where they are most needed and alleviating the psychological burden of uncertainty for entire families.
New Insights into a Different Type of Polyp
In addition to its findings on adenomatous polyps, the study also provided valuable insights into a different and common type of growth known as the serrated polyp. Among approximately sixty individuals in the study cohort who had this type of polyp, the researchers discovered a consistent genetic signature. They found that almost all of these growths contained a non-hereditary mutation in the BRAF gene. This finding is significant because it points to a distinct biological pathway for the development of serrated polyps compared to their adenomatous counterparts. A detailed genetic analysis further revealed that these BRAF-mutated serrated polyps bear a striking resemblance to a simple overgrowth, or hyperplasia, of normal intestinal tissue. This molecular similarity suggests that their origin and potential for progression may be fundamentally different from other polyps that are more clearly on the path to becoming cancerous. The consistent presence of this specific, non-hereditary mutation provides a key biological marker for this polyp subtype.
The discovery that these serrated polyps are genetically similar to benign tissue overgrowth has important clinical implications. Lead researcher Richarda de Voer emphasized that this finding warrants further investigation, as it is not yet clear whether these specific types of polyps will invariably progress to colorectal cancer. While all polyps are generally monitored due to their cancer potential, this research suggests that the risk associated with BRAF-mutated serrated polyps might be different from others. Future studies will be needed to determine the long-term outcomes for patients with these specific growths and to establish whether they require the same intensive surveillance as other polyp types. This line of inquiry could eventually lead to more nuanced screening and management guidelines, allowing clinicians to differentiate between polyps with a high risk of malignancy and those that are less likely to become cancerous, thereby refining personalized cancer prevention strategies even further.
A Clearer Path Forward in Colorectal Cancer Management
Ultimately, this landmark research provided definitive answers for a large cohort of patients who had long been without a clear diagnosis for their condition. The study powerfully demonstrated the immense added value of integrating advanced DNA analysis of polyp tissue into the standard diagnostic pipeline for individuals with suspected hereditary colorectal cancer across Europe. By successfully identifying previously hidden conditions like APC mosaicism, this innovative approach enabled more accurate risk prediction and fundamentally changed how genetic risk is communicated within families. It prevented the need for unnecessary screening for low-risk relatives and provided a much clearer picture of heritable risk for future generations. The findings represented a significant and tangible step forward in the personalized management of colorectal cancer, transforming a diagnostic gray area into one with clear, actionable insights that directly improved patient care and family counseling. The integration of this technique has already begun to reshape clinical practice.