The realm of hemophilia treatment is witnessing a transformative wave, with innovative therapies challenging the status quo of managing this genetic blood clotting disorder, which has burdened patients for decades with frequent infusions to replace missing clotting factors. Now, a newly approved RNA interference (RNAi) drug named Qfitlia, alongside advancements in gene therapy, is igniting hope for a less invasive and more effective future. Could this novel drug, with its promise of fewer doses, become a cornerstone in redefining care for those affected by hemophilia A and B? This exploration delves into the potential of Qfitlia to reshape treatment paradigms while examining the broader landscape of gene therapies that aim for a one-time fix. Despite the excitement, significant obstacles—ranging from scientific limitations to deep-seated patient caution—cast a shadow over these advancements. The journey of these therapies reveals a delicate balance between groundbreaking science and practical challenges, prompting a closer look at how far the field has progressed and what hurdles remain on the path to a true revolution in hemophilia management.
The Emergence of QfitliA Game-Changing Approach
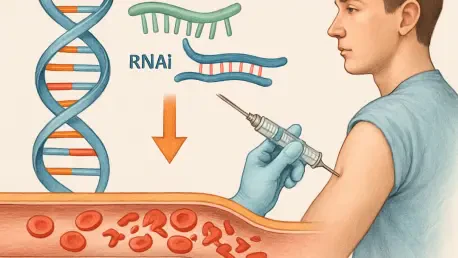
A significant milestone in hemophilia care arrived with the FDA approval of Qfitlia, an RNAi drug, on March 28 of this year. This therapy introduces a distinct mechanism by targeting and reducing a key anticoagulant in the bloodstream, effectively restoring a balance that prevents excessive bleeding without the need to directly replace missing clotting factors VIII or IX. Experts in the field have noted that this approach could alleviate the burden of frequent treatments, a persistent challenge for patients accustomed to regular infusions. The appeal of Qfitlia lies in its potential to simplify regimens, offering a glimpse of a life less tethered to medical schedules. As this drug enters clinical practice, it sparks curiosity about whether it can deliver consistent results across diverse patient populations and stand as a viable alternative to existing options.
Beyond its innovative mechanism, Qfitlia’s arrival signals a shift toward diversifying therapeutic strategies in hemophilia management. Unlike gene therapies that aim for a permanent solution by introducing functional genes, this RNAi drug focuses on rebalancing the body’s natural processes with fewer interventions. Such a design could resonate with patients who prioritize convenience while still seeking reliable protection against bleeds. Additionally, its introduction raises questions about how it will integrate into a healthcare landscape already navigating the complexities of high-cost treatments. The potential for Qfitlia to reduce treatment frequency might not only improve quality of life but also influence how providers and payers evaluate its long-term value compared to other therapies currently in use.
Gene Therapy: Triumphs and Persistent Challenges
Gene therapy has emerged as a beacon of hope for hemophilia B patients, particularly with the success of Hemgenix, a treatment approved several years ago. This therapy has demonstrated remarkable efficacy by achieving stable clotting factor IX levels, often eliminating the need for ongoing treatments and drastically reducing bleeding episodes. Medical professionals have described it as transformative, with many patients experiencing a newfound freedom from the constant fear of uncontrolled bleeds. The stability offered by Hemgenix underscores the potential of gene therapy to redefine what it means to live with hemophilia B, pushing the boundaries of what was once thought possible in managing this condition. However, its high cost and complex administration continue to limit widespread adoption.
In stark contrast, the outlook for hemophilia A patients with gene therapy, specifically Roctavian, tells a more sobering story. While initially promising with high factor VIII levels post-treatment, the efficacy of Roctavian diminishes over time, often leaving patients with levels far below the threshold needed for a bleed-free life. This decline stems from a biological mismatch—liver cells targeted by the therapy are not naturally suited to produce factor VIII, unlike their role in factor IX production for hemophilia B. Ongoing research into alternative delivery methods, such as CRISPR technology and lipid nanoparticles, aims to address this limitation. Despite these setbacks, the field remains optimistic that future innovations will bridge the efficacy gap and offer hemophilia A patients a comparable breakthrough to that seen with Hemgenix.
Shadows of History: Patient Reluctance to Innovate
The hemophilia community’s hesitancy to embrace new therapies is deeply rooted in a painful history that continues to shape perceptions of medical advancements. Decades ago, during the 1970s and 1980s, contaminated factor concentrates derived from pooled plasma led to devastating infections of HIV and hepatitis C among a significant portion of patients with severe hemophilia. This tragic chapter resulted in widespread illness and loss, leaving an indelible mark of caution within the community. Even though current gene therapies and novel drugs like Qfitlia show no evidence of such catastrophic risks, the memory of past harms fuels skepticism. Patients often weigh the uncertainties of long-term side effects against the relative predictability of traditional treatments, slowing the uptake of cutting-edge options.
This reluctance is compounded by the nature of the therapies themselves, which, while promising, do not yet offer a permanent cure. For instance, gene therapies currently lack integration into the patient’s genome, meaning their effects may wane over time, requiring additional interventions. The fear of unknown consequences, coupled with the emotional weight of historical trauma, creates a significant barrier to adoption. Addressing this challenge requires more than scientific progress; it demands transparent communication and robust education efforts to rebuild trust. Only by acknowledging and respecting these concerns can the medical community hope to encourage patients to consider the potential benefits of emerging treatments like Qfitlia and gene therapies.
Systemic Roadblocks: Healthcare’s Struggle to Adapt
Even when patients are willing to explore innovative treatments, the healthcare system often stands as a formidable obstacle to access. Therapies like Hemgenix come with staggering price tags—$3.5 million per dose—placing immense financial strain on institutions unprepared for such expenditures. Hospitals and pharmacies must navigate uncharted territory, developing new safety protocols, training staff on specialized delivery methods, and securing insurance reimbursements that are often delayed or denied. The administrative burden of integrating these therapies into existing frameworks cannot be understated, as it requires a fundamental restructuring of how care is delivered and financed for hemophilia patients.
Moreover, the long-term commitment demanded by these treatments adds another layer of complexity. Institutions must monitor patients for extended periods, potentially up to 15 years, to assess outcomes and manage any delayed effects. This requirement for prolonged follow-up clashes with budget constraints and resource limitations, further complicating adoption. Experts emphasize the need for a dedicated advocate or “champion” within healthcare systems to spearhead the integration of gene therapies and novel drugs like Qfitlia. Without such leadership, the gap between scientific innovation and practical implementation risks widening, leaving many patients unable to access the very treatments that could transform their lives.
The Hidden Costs: Lifestyle and Incomplete Outcomes
Beyond financial and systemic challenges, the personal trade-offs required by advanced hemophilia treatments often temper patient enthusiasm. Gene therapies, for instance, come with strict lifestyle mandates in the initial post-treatment period, such as abstaining from alcohol to protect liver function and using contraception for up to a year. These adjustments, while temporary, can feel burdensome to individuals already managing a chronic condition. Additionally, the intensive monitoring required immediately after treatment adds to the sense of medical oversight, which some patients find intrusive rather than reassuring. Such requirements highlight that even cutting-edge solutions are not without their drawbacks.
Equally significant is the realization that these therapies do not address all aspects of hemophilia’s impact. While they may prevent future bleeding episodes, they cannot reverse pre-existing damage, such as joint deterioration or arthritis caused by past bleeds. This limitation means that for many patients, particularly those with a long history of the condition, the promise of a fully restored quality of life remains out of reach. The gap between preventing future harm and repairing past damage contributes to a cautious “wait-and-see” attitude among both patients and healthcare providers, as they evaluate whether the benefits of therapies like Qfitlia or gene treatments justify the personal and medical compromises involved.
Navigating a Crowded Field: The Future of Treatment Options
The therapeutic landscape for hemophilia is becoming increasingly competitive, with Qfitlia’s entry adding to an array of options that includes gene therapies, bispecific antibodies like Hemlibra, and traditional factor concentrates. This diversity empowers patients and clinicians to tailor treatments to individual circumstances, factoring in efficacy, cost, and lifestyle preferences. However, the abundance of choices also fosters hesitation, as stakeholders often adopt an observational stance, waiting for therapies to mature before making definitive commitments. The dynamic nature of this field suggests that no single approach will dominate in the near term, but rather, a mosaic of solutions will coexist to meet varied needs.
Looking ahead, the interplay between emerging therapies like Qfitlia and established treatments will likely shape the trajectory of hemophilia care. The RNAi drug’s focus on reducing treatment frequency could appeal to those seeking minimal disruption, while gene therapies hold the allure of a potential one-time fix, despite current limitations. Meanwhile, ongoing research into more durable solutions, such as genomic integration or advanced delivery systems, promises to further expand possibilities. As this competitive environment evolves, the emphasis must remain on patient-centered decision-making, ensuring that the benefits of innovation are balanced against practical realities and historical lessons. Only through such a nuanced approach can the field move closer to a true transformation in managing hemophilia.
Reflecting on Progress: Steps Toward a Balanced Future
Looking back, the strides made in hemophilia treatment through gene therapies like Hemgenix have marked a turning point, offering unprecedented relief for many with hemophilia B, while the struggles with Roctavian for hemophilia A underscore persistent scientific challenges. The introduction of Qfitlia as an RNAi drug has brought a fresh perspective, emphasizing convenience through fewer doses and highlighting the diversity of approaches being pursued. Yet, the journey has been far from smooth, as patient caution, systemic barriers, and lifestyle trade-offs temper the pace of adoption. Reflecting on these developments, it becomes clear that bridging the gap between innovation and implementation demands more than breakthroughs in the lab.
Moving forward, the focus should shift to actionable strategies that address these multifaceted hurdles. Enhancing patient education to rebuild trust, advocating for systemic reforms to ease financial and logistical burdens, and accelerating research into more durable therapies stand as critical next steps. Collaboration among researchers, clinicians, and policymakers will be essential to ensure that therapies like Qfitlia and future innovations reach those who need them most. By prioritizing shared decision-making and long-term support, the hemophilia community can navigate this complex landscape with cautious optimism, paving the way for a future where transformative care becomes not just a possibility, but a reality for all.