This how-to guide aims to help readers understand the groundbreaking potential of a novel fusion protein in cancer immunotherapy, providing a detailed roadmap to grasp its development, mechanisms, and implications. By exploring this innovative treatment, the guide equips readers with knowledge about a dual-action therapy that could transform cancer care through targeted immune activation and suppression blockade. The purpose is to break down complex scientific advancements into accessible steps, offering insight into how this molecule may redefine treatment outcomes for patients battling cancer. With a focus on historical context, scientific innovation, and future possibilities, this guide highlights the importance of staying informed about cutting-edge therapies that promise safer and more effective solutions.
The significance of this guide lies in its ability to demystify a major leap forward in medical science at a time when cancer remains a leading cause of death worldwide, with millions of new cases diagnosed each year according to recent global health data. This underscores the urgent need for therapies that go beyond traditional approaches like chemotherapy and radiation. This guide introduces readers to a fusion protein that combines an interleukin-2 variant with a PD-1 antibody, presenting a compelling opportunity to enhance the body’s natural defenses against tumors. By following the outlined steps, readers will gain a comprehensive understanding of how this molecule builds on decades of research to address longstanding challenges in immunotherapy.
Unveiling a Breakthrough in Cancer Treatment
Imagine a world where cancer treatments no longer come with debilitating side effects but instead harness the body’s own immune system with pinpoint accuracy to eradicate tumors. This vision is closer to reality with the emergence of a novel fusion protein, a pioneering therapy that merges two powerful immunotherapy strategies into one targeted approach. This section sets the stage for understanding a development that could significantly improve patient outcomes by reducing toxicity while maximizing effectiveness against cancer cells.
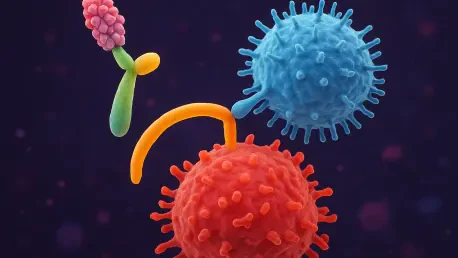
At the heart of this innovation is a dual mechanism that combines an interleukin-2 variant, known as IL-2v, with a PD-1 antibody, creating a synergy that both activates tumor-fighting immune cells and blocks the defenses tumors use to evade attack. This fusion protein represents a potential game-changer in the medical field, promising a safer alternative to existing treatments that often impact healthy tissues. The excitement surrounding this advancement lies in its ability to focus immune responses directly at the tumor site, a feat that could redefine how cancer is managed.
To fully appreciate the impact of this molecule, the following sections will explore its historical roots in immunotherapy, the detailed science behind its components, key research findings, and the broader implications for future treatments. Readers are guided through a journey from past challenges to present innovations, with a clear view of how this therapy might shape the landscape of cancer care. Each step builds a foundation for understanding why this development holds such transformative potential.
The Evolution of Cancer Immunotherapy: From Past to Present
Tracing the origins of immunotherapy reveals a remarkable story of persistence and progress that began with a historic case in the 1980s, when a young woman named Linda Taylor, diagnosed with advanced skin cancer, became the first patient to be cured through this innovative approach. Under the expertise of Dr. Stephen Rosenberg at a leading research institute, her treatment with interleukin-2 (IL-2), a molecule that stimulates immune cells to attack tumors, marked a turning point, demonstrating that the body’s defenses could be weaponized against cancer.
The approval of IL-2 as the first immunotherapy drug by regulatory authorities shifted the paradigm of cancer treatment, moving away from solely relying on surgery or toxic chemicals. However, despite its groundbreaking success, IL-2 therapy revealed significant drawbacks, including severe side effects caused by its non-specific activation of immune cells across the body. Additionally, its unintended stimulation of regulatory T cells, which suppress immune activity, often diminished the desired anti-tumor response, posing a challenge for widespread application.
These limitations spurred decades of research aimed at refining immunotherapy to enhance precision and safety, ultimately leading to the creation of the fusion protein at the center of this guide. Scientists sought to address the systemic toxicity and counteractive immune suppression that plagued early IL-2 treatments. This historical context underscores the importance of the new molecule as a culmination of persistent efforts to improve upon foundational therapies, paving the way for more targeted and tolerable options in cancer care.
Understanding the Fusion Protein: A Dual-Action Innovation
Delving into the science of the fusion protein offers a glimpse into how it integrates two distinct mechanisms to combat cancer with unprecedented precision, pairing an IL-2 variant engineered for selective immune activation with a PD-1 antibody that blocks tumor defenses. The result is a therapy designed to maximize impact at the tumor site while minimizing harm to healthy tissues.
The dual-action approach leverages the strengths of both components to create a synergistic effect, addressing multiple barriers that tumors use to resist immune attacks. By focusing on specific immune pathways, this fusion protein stands out from traditional therapies that often cast a wider, less controlled net. This section breaks down each element to provide clarity on how they work together to enhance treatment efficacy.
The following subsections detail the individual roles of the IL-2 variant and PD-1 antibody, as well as their combined power in targeting cancer. Understanding these mechanisms is crucial for appreciating the potential of this therapy to outperform existing options. Each component contributes uniquely to a comprehensive strategy that could set a new standard in immunotherapy.
Component 1: IL-2 Variant for Selective Immune Activation
The IL-2 variant, or IL-2v, represents a refined version of the original IL-2 molecule, tailored to activate only those immune cells directly involved in fighting tumors. Unlike its predecessor, which triggered broad immune responses, IL-2v is designed to avoid stimulating regulatory T cells that can dampen the body’s anti-cancer efforts. This selective approach marks a significant improvement in controlling immune activity.
By focusing on tumor-killing cells, IL-2v ensures that the immune response is directed where it is most needed, reducing the risk of widespread inflammation or toxicity. This precision addresses the historical challenges faced by IL-2 therapies, which often led to severe side effects due to non-specific activation. The modification of this molecule reflects a deeper understanding of immune dynamics in cancer treatment.
Targeted Stimulation: Enhancing Tumor-Fighting Power
Targeted stimulation through IL-2v prioritizes the activation of relevant immune cells, such as cytotoxic T cells, which are critical for destroying cancer cells. This focused approach contrasts sharply with older methods that inadvertently activated irrelevant or suppressive cell types, diluting the therapeutic effect. The result is a more potent and efficient attack on tumors without the collateral damage seen in earlier treatments.
This specificity not only enhances the tumor-fighting power but also contributes to a safer treatment profile for patients. By limiting immune activation to the necessary players, the therapy avoids overwhelming the body’s systems, a common issue in past immunotherapies. Such advancements highlight the potential for IL-2v to redefine how immune responses are harnessed in clinical settings.
Component 2: PD-1 Antibody to Block Tumor Defenses
Complementing the IL-2v, the PD-1 antibody component targets a key mechanism that cancer cells exploit to evade immune detection. Tumors often express signals that bind to the PD-1 receptor on immune cells, effectively sending a “do not attack” message that halts immune activity. The antibody blocks this interaction, releasing the brakes on the immune system to allow a full-scale assault on the tumor.
This blockade is essential for overcoming the natural defenses that tumors develop to shield themselves from immune responses, ensuring that the body’s protective mechanisms are not hindered. By neutralizing the inhibitory pathway, the PD-1 antibody allows activated immune cells to perform their role without interference. This mechanism has proven effective in various existing therapies but gains new strength when combined with targeted immune stimulation.
Overcoming Suppression: Disabling Cancer’s Shield
Disabling cancer’s shield through PD-1 antibody action directly tackles the suppressive microenvironment surrounding tumors, which often renders immune cells ineffective by signaling them to stand down. This allows cancer to grow unchecked, but the antibody’s role is to disrupt this barrier, enabling a sustained and aggressive immune response at the tumor site.
The impact of overcoming suppression lies in restoring the body’s ability to recognize and attack cancer as a threat, which is essential for effective treatment. This step is crucial for ensuring that immune cells, once activated, are not immediately neutralized by tumor defenses. Such a targeted intervention enhances the overall effectiveness of immunotherapy by addressing a critical obstacle in tumor biology.
Synergy in Action: Combining Forces for Greater Impact
The true strength of the fusion protein emerges from the synergy between IL-2v and the PD-1 antibody, creating a multifaceted immune response that targets cancer effectively. The antibody guides the IL-2v directly to the tumor microenvironment, ensuring that immune activation occurs where it matters most. Simultaneously, it blocks suppressive signals, allowing the activated cells to operate at full capacity against cancer.
This combined approach results in a treatment that is greater than the sum of its parts, tackling both immune activation and suppression in a coordinated manner. Unlike single-mechanism therapies, this fusion protein addresses multiple aspects of tumor evasion, increasing the likelihood of a durable response. The integration of these strategies represents a forward-thinking solution in cancer treatment design.
Precision Delivery: Minimizing Side Effects
Precision delivery is a hallmark of this fusion protein, focusing immune activation at the tumor site to minimize systemic side effects. By directing IL-2v to specific areas through the guidance of the PD-1 antibody, the therapy avoids the widespread immune stimulation that often leads to toxicity in traditional treatments. This targeted method offers a safer alternative for patients undergoing immunotherapy.
Reducing off-target effects is a critical advantage, as it lowers the risk of severe reactions that can compromise patient health and treatment continuation. The ability to concentrate therapeutic action where it is needed most demonstrates a significant leap in controlling the scope of immune responses. Such precision could become a cornerstone of future cancer therapies, prioritizing patient safety alongside efficacy.
Key Research Findings: Promising Preclinical Results
Preclinical studies provide compelling evidence of the fusion protein’s potential, offering valuable insights into its effectiveness against cancer. Research led by Professor Alfred Zippelius at a prominent university utilized samples from lung cancer patients to test the therapy’s impact on immune cells within tumors. The results highlight the molecule’s ability to achieve targeted and potent anti-cancer effects.
These studies underscore the importance of validating new therapies through rigorous experimentation before advancing to human trials. The findings not only demonstrate the fusion protein’s promise but also identify specific advantages over existing treatments. This section explores two key outcomes that emerged from the research, shedding light on how this therapy could address critical challenges in immunotherapy.
A deeper look into the data reveals the fusion protein’s capacity to transform immune responses within the tumor microenvironment, highlighting its potential as a groundbreaking approach in medical research. These preclinical successes lay the groundwork for further development, providing a strong rationale for ongoing clinical evaluations. Understanding these results is essential for appreciating the therapy’s potential impact on cancer care.
Finding 1: Selective Activation of Tumor-Killing Cells
One of the standout findings from the preclinical studies is the fusion protein’s ability to selectively activate immune cells capable of targeting and destroying cancer. Unlike traditional IL-2 therapies, which activate a broad range of cells, this treatment focuses solely on tumor-killing cells, avoiding regulatory T cells that suppress immune activity. This selectivity is a pivotal advancement in enhancing treatment specificity.
Such targeted activation ensures that the immune response is not diluted or counteracted by cells that hinder anti-tumor efforts. The research demonstrated a clear preference for engaging the right immune players, resulting in a more effective attack on cancer cells within patient samples. This outcome points to a therapy that could outperform older methods by maintaining a focused immune assault.
Specificity Advantage: A Focused Attack
The specificity advantage of this therapy lies in its capacity to mount a focused attack on tumors without triggering unnecessary immune activity. By sidestepping regulatory T cells, the fusion protein sustains a robust anti-cancer response that is not easily diminished. This precision offers a marked improvement over past immunotherapies that struggled with maintaining effective immune engagement.
A focused attack translates to better outcomes for patients, as it concentrates therapeutic power where it is most needed, enhancing the likelihood of tumor reduction and control. The ability to avoid counterproductive immune suppression further improves these results. This aspect of the fusion protein’s design could set a new benchmark for how immunotherapy targets cancer with accuracy and efficiency.
Finding 2: Reawakening Exhausted Immune Cells
Another critical finding from the research is the fusion protein’s ability to reawaken exhausted immune cells within the tumor microenvironment. These cells, often rendered inactive due to prolonged exposure to suppressive tumor signals, lose their capacity to fight cancer effectively. The therapy revitalizes them by blocking inhibitory pathways and providing targeted stimulation.
This reawakening is a breakthrough in addressing a major barrier to successful immunotherapy, as immune exhaustion frequently undermines treatment efforts. The preclinical data showed that once revitalized, these cells regained their tumor-fighting capabilities, contributing to a stronger overall immune response. Such restoration is vital for tackling persistent or resistant cancers that evade standard therapies.
Restoring Vigor: Combating Immune Exhaustion
Restoring vigor to exhausted immune cells is a key mechanism for combating immune exhaustion, a common challenge in cancer progression. By reversing the inactivity caused by tumor suppression, the fusion protein enables these cells to resume their critical role in attacking cancer. This restoration process amplifies the body’s natural defenses in a way that single-mechanism therapies often cannot achieve.
The significance of combating exhaustion lies in its potential to extend the effectiveness of immune responses over time, offering hope for better cancer management. Tumors rely on wearing down immune cells to maintain growth, but this therapy disrupts that strategy by reinvigorating the body’s fighters. This capability could prove essential for achieving lasting control over cancer, particularly in advanced or recurring cases.
Advantages and Potential Impact: A Step Beyond Current Therapies
The fusion protein offers distinct advantages that position it as a significant step beyond current immunotherapies, addressing limitations that have long hindered effective treatment. Its targeted action focuses the immune response directly at the tumor site, drastically reducing the systemic side effects associated with traditional IL-2 therapies. This precision minimizes the risk of toxicity, a common issue that often forces patients to discontinue treatment.
Another key benefit is the dual mechanism, which combines immune activation through IL-2v with suppression blockade via the PD-1 antibody, providing a comprehensive approach to combating cancer. Additionally, selective activation ensures that regulatory T cells are bypassed, maintaining a sustained anti-tumor response without counterproductive suppression. Compared to single-agent therapies, this fusion protein tackles multiple facets of tumor evasion simultaneously.
The potential impact of these advantages is profound, as they suggest a redefinition of cancer care standards. By outperforming older IL-2 treatments and standalone checkpoint inhibitors, this therapy could offer patients a more tolerable and effective option. Such improvements highlight the possibility of shifting immunotherapy toward more personalized and efficient strategies, ultimately improving survival rates and quality of life for those affected by cancer.
Looking Ahead: Clinical Trials and Broader Trends
Currently, the fusion protein is under evaluation in phase I clinical trials led by a major pharmaceutical company, focusing on safety and dosing assessments in human subjects. These early-stage trials, initiated in recent years, are crucial for determining whether the promising preclinical results translate to real-world patient benefits. The outcomes will shape the therapy’s path forward, potentially confirming its role as a cornerstone in cancer treatment.
Future developments may include tailoring this therapy for personalized approaches, aligning with individual tumor profiles and immune characteristics to maximize effectiveness. Beyond its immediate application, the fusion protein could inspire other combination therapies, integrating multiple mechanisms into single treatments for various diseases. Such innovations reflect a growing trend in immunotherapy toward precision and multi-faceted strategies that address the complexity of cancer biology.
Broader challenges, such as cost and accessibility, remain considerations as this therapy advances through clinical stages. Ensuring that cutting-edge treatments reach diverse patient populations is essential for equitable impact. As research progresses from the current year to future milestones, the fusion protein’s success could catalyze a shift in how cancer care prioritizes integrated, patient-centered solutions within the evolving landscape of medical science.
Final Thoughts on a New Hope for Cancer Immunotherapy
Reflecting on the journey through this guide, the exploration of the fusion protein’s development has illuminated a path from historical immunotherapy challenges to a dual-action innovation that tackles selective immune activation and suppression blockade. The detailed steps have broken down its mechanisms, from IL-2v’s targeted stimulation to the PD-1 antibody’s role in disabling tumor defenses, alongside preclinical evidence that showcases its potential to transform cancer treatment. Each aspect has contributed to a clearer picture of how this therapy aims to reduce side effects while enhancing efficacy.
Looking beyond what has been covered, the next steps for stakeholders involve closely monitoring the outcomes of ongoing clinical trials to assess real-world applicability. For those invested in cancer care advancements, staying updated on trial results and advocating for accessible implementation have emerged as critical actions. Additionally, exploring parallel research into combination therapies has offered a promising avenue to amplify the impact of such innovations, ensuring that the momentum built by this fusion protein continues to drive progress in defeating cancer.