In the realm of breast cancer research, Ivan Kairatov stands out as a biopharma expert bringing innovative insights to the understanding of tumor dynamics. Our conversation today centers around a groundbreaking study from Fox Chase Cancer Center, which deeply examines tumor growth rates and the implications of surgical delays on breast cancer staging. This dialogue touches upon the nuanced relationship between clinical and pathologic tumor assessments and the broader impact of these findings on patient care and future research.
Can you explain the novel method used to analyze tumor growth rates in the study?
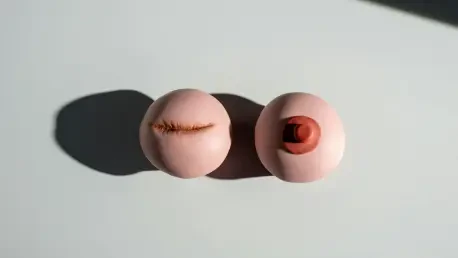
The study introduces a pioneering approach by utilizing pathologic tumor sizes, rather than relying solely on clinical measurements like imaging results, which are often less precise. By comparing the size of the tumor at the time of surgery to what was initially determined through clinical imaging, researchers could better understand how much a tumor grows during the wait for surgery. This method provides a more refined analysis of tumor growth and helps in accurately assessing the progression of the cancer.
What specific insights does the study provide about breast tumor progression between diagnosis and surgery?
This research offers crucial insights into how breast tumors evolve between the initial diagnosis and the surgical intervention. It quantifies growth rates for tumors of varying sizes and characteristics, providing both patients and physicians with a clearer picture of the growth potential within that waiting period. It essentially equips them with data-driven peace of mind, as the growth is often not as rapid as feared, which can help in making informed decisions about the timing of surgery.
Why is pathologic tumor size considered more accurate than clinical size?
Pathologic tumor size is regarded as more reliable because it is based on the actual examination of the tumor post-removal. Clinical size, on the other hand, is derived from imaging tools like CT scans or X-rays, which can sometimes be imprecise due to factors like the imaging resolution and the interpretation of results. Thus, the pathologic assessment removes a layer of uncertainty by providing a direct measurement.
How can the study’s findings alleviate patients’ concerns about tumor growth while waiting for surgery?
The study reveals that the actual risk of significant tumor growth or spreading (upstaging) during surgical delays is much lower than many patients fear. By demonstrating that the rate of upstaging remains low, even with months-long delays, it reassures patients that immediate surgical intervention may not always be critical. This knowledge can significantly reduce anxiety as patients understand that their window for successful treatment is broader than they might have assumed.
Could you elaborate on the relationship between surgical delays and breast cancer staging?
Surgical delays are often seen with apprehension, but this study provides evidence that these delays might not necessarily lead to significant changes in cancer staging. Staging quantifies how much cancer has spread, and while delay may naturally provoke concern about progression, the study underscores that the risk of considerable upstaging remains minimal over reasonable waiting periods.
What does “upstaging” mean in the context of breast cancer, and how does it relate to surgical delays?
Upstaging occurs when cancer is found to be more advanced during surgery than was initially diagnosed. This research highlights that concerns about upstaging due specifically to surgical delays may be overstated, as many instances of upstaging actually stem from initial inaccuracies in clinical staging, rather than from the cancer spreading during the wait for surgery.
How did the inaccuracies in clinical staging contribute to the observed upstaging in the study?
The study found that clinical staging, which is based on imaging, might not always accurately reflect the true extent of cancer. These inaccuracies can cause what appears to be cancer progression by the time of surgery, whereas it’s often simply a case of more precise measurement by the pathologic process revealing the actual size and spread of the cancer.
What data source did the researchers use, and what was the size and scope of the dataset?
Researchers drew from the National Cancer Database, a robust repository comprising over a million breast cancer patient records collected from 2010 to 2020. This extensive dataset allowed the study to provide statistically significant insights into tumor dynamics and surgical outcomes, making the findings widely applicable.
How do the study’s findings compare with previous data on surgical delays and mortality risks?
Prior studies suggested a correlation between surgical delays and increased mortality risks, though this study refines that understanding by showing single-digit mortality risks even with surgical delays extending several months. This nuanced view indicates that while timely surgery is advisable, moderate delays might not have been as detrimental as previously believed.
How can this study help refine diagnostic tools and clinical assessments in the future?
The findings highlight the importance of improving imaging and initial clinical assessment techniques to reduce staging inaccuracies. By investing in advanced diagnostic technologies and methodologies, the medical community can enhance early-stage evaluation accuracy, ultimately leading to more effective treatment planning and reduced risks of upstaging at surgery.
What implications do these findings have for physicians advising patients about treatment timelines?
With these insights, physicians can have more informed discussions with patients about the timing of their surgeries. Understanding that moderate delays have a minimal impact on staging, doctors can prioritize cases more efficiently without compromising care quality, avoiding unnecessary stress over the timing of surgeries.
In what ways can this research empower patients dealing with a breast cancer diagnosis?
Armed with the information from this study, patients can make decisions with greater confidence. Knowing that a delay in surgery doesn’t necessarily lead to a worse prognosis, they can better balance treatment urgency with personal circumstances and preferences, contributing to a more patient-centered approach to care.
How do you foresee the medical community using this information to improve patient outcomes?
Moving forward, this study paves the way for enhanced patient education and more nuanced surgical scheduling. The findings could lead to changes in clinical guidelines and protocols, ultimately aiming to maintain high standards of care while reducing unnecessary stress for patients during what is undoubtedly a difficult time.