A profound shift in understanding the genetic roots of hypermobile Ehlers–Danlos syndrome is underway, as a landmark study dismantles the long-standing theory of a single-gene cause for this complex and often debilitating condition. For decades, the search for a solitary genetic culprit has left patients, clinicians, and researchers with more questions than answers. Now, pioneering research not only provides a compelling new explanation for the disorder’s genetic architecture but also charts a new course for diagnosis and treatment, offering a beacon of hope to a community long navigating in the dark. This work suggests that the answer lies not in one faulty gene, but in a complex symphony of genetic variations playing out across multiple biological systems.
Challenging the Single-Gene Paradigm in hEDS
The central thesis of this new research directly confronts the prevailing belief that hypermobile Ehlers–Danlos syndrome (hEDS), like its rarer counterparts, originates from a single gene mutation. For years, the scientific community has approached hEDS with a monogenic lens, a strategy that has consistently failed to yield a definitive cause. This study boldly reframes the condition as a polygenic disorder, where an accumulation of multiple, subtle genetic variants collectively contributes to the clinical presentation. This shift in perspective is not merely academic; it represents a fundamental re-evaluation of the disorder’s biological basis, moving away from a model that has proven inadequate.
This new framework emerged from the necessity to solve a persistent problem: the failure of countless previous studies to identify a causative gene for the most common form of EDS. While other types of Ehlers–Danlos syndrome have been linked to specific genes, hEDS has remained a frustrating enigma. The inability to pinpoint a single gene has created a significant barrier to developing reliable diagnostic tests and targeted therapies. By proposing a polygenic model, the researchers provide a plausible explanation for this “missing heritability” and establish a more complex but ultimately more accurate understanding of the condition’s genetic landscape.
The Clinical and Genetic Enigma of Hypermobile EDS
Hypermobile Ehlers–Danlos syndrome is widely recognized as a prevalent heritable connective tissue disorder, affecting an estimated 1% to 3% of the population and accounting for up to 90% of all EDS cases. Despite its frequency, the condition is notoriously underdiagnosed, largely due to a lack of awareness within the medical community and the absence of a definitive molecular diagnostic tool. Patients often endure a prolonged and frustrating diagnostic odyssey, facing years of uncertainty and misdiagnosis while navigating a complex array of symptoms that impact nearly every system in the body.
The critical importance of this research is underscored by the severe and multi-systemic nature of the condition. The hallmark of hEDS is generalized joint hypermobility, leading to chronic pain, instability, and frequent dislocations. However, its effects extend far beyond the joints, causing skin hyperextensibility, tissue fragility, poor wound healing, and a host of associated conditions, including profound fatigue and autonomic dysfunction. The development of a genetic test is not just a matter of convenience; it is a crucial step toward validating patients’ experiences, enabling early intervention, and preventing misinterpretations, such as the devastating misdiagnosis of child abuse in cases of unexplained fragility fractures.
Research Methodology Findings and Implications
Methodology
To unravel this genetic puzzle, the research team adopted a pioneering approach that powerfully integrates advanced machine learning algorithms with deep genomic analysis. By leveraging computational tools like random forest algorithms and deep neural networks, the scientists were able to sift through immense volumes of genetic data to identify subtle patterns that traditional statistical methods would likely miss. This innovative strategy allowed for a more holistic analysis, capable of detecting the cumulative effect of many small genetic variations rather than searching for a single, powerful mutation.
The study’s foundation was a meticulously designed analysis of 116 individuals from 43 families, which included both patients clinically diagnosed with hEDS and their unaffected relatives who served as a control group. Using Whole Exome Sequencing (WES), the researchers examined the protein-coding regions of the genome for each participant, generating a massive dataset of tens of thousands of rare genetic variants. This family-based design, combined with the sophisticated machine learning framework, enabled the team to effectively isolate the genetic signals specifically associated with the presence of hEDS, providing a clear and statistically robust path toward their groundbreaking findings.
Findings
The study’s primary discovery was a clear and significant difference in the genetic makeup of individuals with hEDS compared to their unaffected family members. The analysis revealed that hEDS patients carry a much higher “burden of variants”—a greater accumulation of potentially disruptive genetic changes—than the controls. This finding provides the first strong, data-driven evidence that hEDS is not caused by a single gene but is instead a polygenic disorder, where the combined impact of many variants pushes an individual over a threshold toward developing the condition.
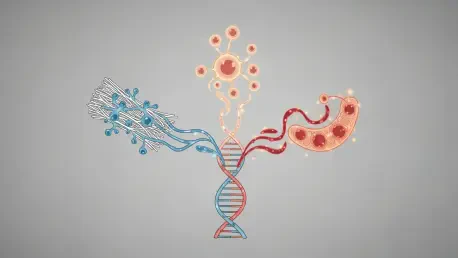
Furthermore, the machine learning models pinpointed three distinct biological systems where these genetic variations were predominantly clustered. The first is the Collagen Biosynthesis Pathway, which aligns with the classic understanding of EDS as a connective tissue disorder. The second, a more novel finding, is the HLA/Adaptive Immune Axis, suggesting that immune system dysregulation may play a key role in the disorder’s pathology, potentially explaining inflammatory symptoms. The third is the Mitochondrial Respiratory Chain, which governs cellular energy production; variations here could account for the pervasive fatigue and poor tissue repair commonly reported by patients.
Implications
The transformative potential of these findings is immense. By identifying a multi-system genetic signature, this research lays the essential groundwork for developing the first comprehensive genetic test for hEDS. Such a diagnostic tool would revolutionize patient care, dramatically shortening the diagnostic odyssey and providing definitive answers for countless individuals and families. A reliable test would also facilitate more accurate genetic counseling, helping families understand inheritance patterns and risks for future generations.
Beyond diagnostics, the identification of three target biological systems opens exciting new avenues for therapeutic intervention. Understanding the roles of collagen, immune, and mitochondrial pathways in hEDS allows for the exploration of precision medicine and the development of tailored treatment strategies. Instead of a one-size-fits-all approach to symptom management, future therapies could be designed to address an individual’s specific genetic vulnerabilities, offering the promise of more effective and personalized care.
Reflection and Future Directions
Reflection
It is important to clarify that these findings represent strong genetic associations that now require further validation to be confirmed as direct causative mechanisms. The study has successfully identified high-priority candidate genes and pathways, but the journey from association to causation involves additional layers of functional research. The results provide a robust and evidence-based roadmap for the scientific community, guiding future investigations toward the most promising areas.
A primary challenge in this research was navigating the sheer scale and complexity of genomic data. Analyzing tens of thousands of variants across more than a hundred individuals presented a significant analytical hurdle. The successful application of an integrated machine learning approach was critical to overcoming this obstacle. This novel methodology proved adept at discerning the subtle, cumulative signals of a polygenic disorder from the background noise of normal human genetic variation, demonstrating its power in contexts where traditional approaches have fallen short.
Future Directions
The immediate next steps for research involve in-depth functional studies to confirm the causative roles of the identified genetic variants. Scientists will need to investigate how these specific variations impact cellular processes within the collagen, immune, and mitochondrial systems to understand their precise biological effects. These follow-up experiments are essential to fully elucidate the molecular pathophysiology of hEDS and to translate the genetic findings into concrete clinical applications.
Looking ahead, the methodological framework developed in this study holds significant promise for the broader field of rare disease genetics. The integrated machine learning approach provides a powerful template for tackling the “missing heritability” problem in other genetically complex disorders that have long eluded explanation. By applying this model, researchers may be able to unlock the genetic secrets of numerous other conditions, paving the way for new diagnostics and therapies across the rare disease spectrum.
Conclusion A New Horizon for hEDS Diagnosis and Treatment
This landmark study successfully repositioned hypermobile Ehlers–Danlos syndrome as a complex, polygenic disorder, marking a pivotal moment for patients and researchers alike. The evidence clearly pointed to a multi-system condition, with genetic vulnerabilities converging across collagen biosynthesis, immune regulation, and mitochondrial function. This revelation not only explained decades of frustrating results from single-gene inquiries but also provided a clear, evidence-based path forward.
The research’s contribution extended beyond a new understanding of hEDS; it offered a powerful methodological blueprint for investigating other genetically elusive rare diseases. By demonstrating the efficacy of integrating advanced machine learning with genomic analysis, the study has equipped the scientific community with a new tool to solve some of genetics’ most persistent mysteries. The work has fundamentally altered the trajectory of hEDS research, ushering in an era of renewed hope for the development of definitive diagnostics and targeted, personalized therapies that the Ehlers–Danlos community has long awaited.