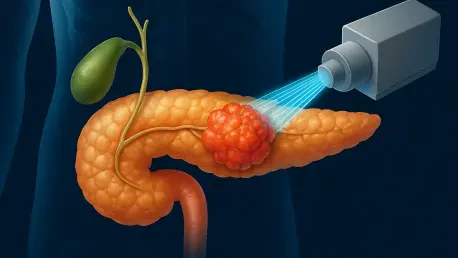
Pancreatic cancer remains one of the most devastating diagnoses a patient can receive, with survival rates that have barely improved in decades and a prognosis that often leaves little room for hope. Among the various forms of this disease, pancreatic ductal adenocarcinoma (PDAC) stands out as the most common and aggressive, accounting for about 90% of cases. Each year, thousands are affected, with over 10,000 new diagnoses in the UK alone, and sadly, more than 9,000 deaths. Despite advances in medical science, only 5% of patients survive beyond ten years, underscoring the urgent need for innovative treatments. A recent discovery by scientists at The Institute of Cancer Research in London offers a glimmer of promise, identifying a critical protein that could change the trajectory of this deadly disease. This finding paves the way for potential therapies that might prevent the cancer from spreading, addressing one of the primary reasons for its lethality. The implications of this research could mark a turning point in how PDAC is managed, offering renewed focus on targeted interventions.
Unveiling a Key Player in Cancer Progression
A pivotal element of this groundbreaking research centers on a protein known as SPP1, which has been linked to the aggressive spread of PDAC. Published in a prestigious scientific journal, the study analyzed tumor data from 644 patients, revealing a stark correlation between elevated SPP1 levels and poorer survival outcomes. The protein appears to play a significant role in enabling cancer cells to metastasize, spreading to vital organs and worsening the disease’s impact. This discovery is not just a statistical observation but a potential game-changer, as it highlights a specific target for therapeutic intervention. By understanding how SPP1 influences cancer progression, researchers have opened a door to developing treatments that could halt the disease in its tracks. The urgency to address pancreatic cancer’s dismal prognosis fuels this work, emphasizing the critical need for solutions that go beyond traditional approaches and focus on the molecular drivers of the disease.
The research took a deeper dive into SPP1’s effects by employing advanced experimental models, such as pancreatic cancer organoids—miniature lab-grown tumors that replicate the behavior of cancer cells in the human body. When the gene responsible for producing SPP1 was deactivated in these models, the results were striking: tumor growth was significantly reduced, with fewer and smaller tumors forming. Moreover, the presence of aggressive cancer cells capable of invading new tissues and migrating was notably diminished. This finding suggests that SPP1 is not merely a bystander but a key facilitator of the cancer’s deadly spread. In parallel, the study explored how this protein interacts with the tumor environment, providing insights into why some cases of PDAC become so resistant to treatment. These experimental outcomes lay a robust foundation for believing that targeting SPP1 could transform the management of this challenging cancer.
Promising Results from Preclinical Trials
Further validation of SPP1’s role came through preclinical trials involving mouse models of PDAC, where the impact of disabling the SPP1 gene was nothing short of remarkable. In mice with the active gene, none survived beyond 50 days, while 20% of those without it lived up to 400 days—a dramatic extension of life. Even more compelling was the absence of cancer spread to the liver or lungs in mice lacking SPP1, compared to significant metastasis rates in those with the gene active. This stark contrast underscores the protein’s influence on the disease’s ability to metastasize, a primary factor in its high mortality rate. Such findings provide a compelling case for pursuing therapies that can block SPP1, potentially altering the course of PDAC for countless patients. The success in these models highlights a tangible path forward, bridging the gap between laboratory research and real-world application.
Beyond genetic deactivation, the research team tested the effects of blocking SPP1 with an antibody in mouse models, yielding equally encouraging results. Half of the treated mice survived beyond 100 days, a significant improvement over the mere 30 days for untreated counterparts. Additionally, the antibody effectively prevented the cancer from spreading, reinforcing the idea that SPP1 is a linchpin in metastasis. This approach offers a glimpse into how future treatments might be designed, using targeted antibodies or similar agents to neutralize the protein’s harmful effects. The consistency of these outcomes across different experimental setups strengthens the argument for SPP1 as a viable drug target. As the scientific community looks to translate these findings into clinical therapies, the potential to curb one of the deadliest aspects of pancreatic cancer becomes increasingly tangible, providing a beacon of hope for those affected by this relentless disease.
Building on Molecular Insights
The study also connects SPP1 to another protein, GREM1, previously identified by the same research team as a factor in PDAC aggressiveness. While low GREM1 levels are associated with increased cancer spread, blocking SPP1 naturally elevates GREM1, keeping cancer cells in a less aggressive and more treatable state. This interplay between the two proteins reveals a complex molecular landscape that governs how pancreatic cancer behaves and progresses. Understanding these relationships is crucial for developing comprehensive treatment strategies that address multiple facets of the disease. The ability to manipulate these molecular pathways offers a nuanced approach to therapy, potentially enhancing the effectiveness of interventions by targeting complementary mechanisms. Such insights are vital for crafting solutions that are not only effective but also sustainable in managing a cancer notorious for its resistance to conventional methods.
This discovery builds on a broader effort to unravel the intricate mechanisms behind pancreatic cancer’s lethality, integrating findings about related proteins to create a fuller picture of the disease. Researchers, including prominent figures from The Institute of Cancer Research, express optimism about the potential of targeting SPP1 to halt PDAC’s spread. Their statements reflect a shared belief that transforming this cancer into a more manageable condition is within reach, provided that drug development efforts build on these preclinical successes. The focus now shifts to designing precise therapeutic agents, such as antibodies or small molecule drugs, that can effectively target SPP1 in human patients. This molecular understanding not only enhances the prospects for better treatments but also underscores the importance of continued investment in research to tackle one of the most challenging cancers known to medicine.
Paving the Way for Future Therapies
Reflecting on the journey of this research, the identification of SPP1 as a driver of pancreatic cancer metastasis marked a significant milestone in the fight against PDAC. The dramatic improvements in survival and reduction in cancer spread observed in preclinical models provided concrete evidence of the protein’s critical role. These experiments, conducted with meticulous attention to detail, laid the groundwork for a new era of targeted therapies that could alter the landscape of pancreatic cancer treatment. The optimism expressed by leading scientists at the time echoed a collective determination to push boundaries and challenge the status quo of stagnant survival rates. Their efforts underscored a pivotal moment when hope began to outweigh despair in the battle against this formidable disease.
Looking ahead, the path forward involves translating these laboratory successes into clinical realities, a process that demands rigorous testing and collaboration across scientific and medical fields. The next steps should focus on developing and trialing drugs that can safely and effectively block SPP1 in humans, potentially revolutionizing how PDAC is treated. Additionally, integrating insights about related proteins like GREM1 could lead to combination therapies that address multiple aspects of cancer progression. As drug discovery efforts advance, the emphasis must remain on precision and patient safety, ensuring that new treatments offer meaningful improvements in quality of life. This research stands as a testament to the power of scientific innovation, offering a roadmap for future breakthroughs that could one day turn a dire diagnosis into a manageable condition.