Neuroblastoma, a devastating cancer affecting primarily children under five, stands as one of the most aggressive solid tumors in pediatric populations, with high-risk cases often showing dismal outcomes despite rigorous treatments. With only about half of these young patients achieving a cure through conventional methods like chemotherapy and radiation, the urgency for novel, less toxic approaches cannot be overstated. This guide delves into best practices surrounding a groundbreaking drug-diet combination that promises to slow tumor growth and transform cancer cells, offering hope for improved survival and quality of life.
The significance of adopting innovative strategies in treating neuroblastoma lies in addressing the severe side effects and limited efficacy of existing therapies. Harsh treatments often leave lasting damage on growing bodies, underscoring the need for gentler, targeted interventions. This guide aims to equip healthcare providers and families with actionable insights into a promising therapeutic approach that prioritizes precision and tolerability.
By focusing on a combination of pharmacological and dietary interventions, this emerging strategy represents a shift toward personalized medicine in pediatric oncology. The following sections outline best practices for understanding and potentially implementing this novel method, drawing from preclinical successes and ongoing research efforts. The goal is to foster informed decision-making and encourage participation in advancing treatment options for affected children.
Understanding the Core Components of the Drug-Diet Approach
Leveraging DFMO to Inhibit Tumor Growth
A cornerstone of this innovative treatment is difluoromethylornithine (DFMO), a drug approved in Switzerland that targets polyamine production, a critical factor in tumor cell proliferation. Best practice involves recognizing DFMO’s role in disrupting uncontrolled cell division by interfering with protein synthesis and genetic translation. Healthcare providers should stay updated on its mechanism to better explain its potential benefits to families of neuroblastoma patients.
Implementing DFMO as part of a therapeutic regimen requires careful monitoring of dosage and patient response, given its novel application in pediatric cancer. Collaboration with oncologists and pharmacologists ensures that administration aligns with the latest research findings, maximizing its impact on slowing tumor progression. This targeted approach minimizes collateral damage to healthy tissues, a significant advantage over traditional therapies.
Integrating a Specialized Diet for Enhanced Outcomes
Complementing DFMO, a proline- and arginine-free diet serves as a vital component by limiting polyamine precursors, thereby amplifying the drug’s effectiveness. A best practice for clinicians and dietitians is to develop tailored nutritional plans that adhere to these restrictions while ensuring the child’s overall health and growth are not compromised. Educating families on dietary adherence is essential for the success of this combined strategy.
To support implementation, multidisciplinary teams should provide resources such as meal plans and counseling to ease the burden of maintaining such a controlled diet. Regular follow-ups can help address challenges and adjust plans as needed, ensuring that nutritional needs are met without undermining therapeutic goals. This dietary intervention, when paired with DFMO, shows potential to not only curb tumor growth but also promote cellular maturation.
Promoting Tumor Cell Maturation as a Therapeutic Goal
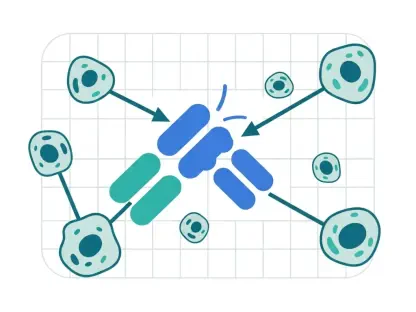
Unlike conventional treatments focused on destroying cancer cells, this approach prioritizes reprogramming them into functional nerve cells, a process disrupted in neuroblastoma. Best practice involves educating medical teams on this paradigm shift, emphasizing cellular transformation over eradication. Such understanding can guide discussions with families about the unique benefits of this method, including reduced toxicity.
Preclinical evidence highlights the drug-diet combo’s ability to encourage cancer cells to mature, offering a less invasive path to treatment. Practitioners should advocate for research participation to further validate these findings, ensuring that the potential for long-term health benefits is thoroughly explored. This focus on maturation represents a forward-thinking strategy in pediatric cancer care.
Translating Preclinical Success to Clinical Application
Building on Promising Preclinical Results
Preclinical trials in mouse models have demonstrated significant success with the DFMO and diet combination, showing slowed tumor growth and, in some instances, regression. A key best practice is for research institutions and clinical teams to prioritize translating these findings into human trials, maintaining rigorous standards for safety and efficacy. Staying informed about these results can help clinicians prepare for future treatment protocols.
The tolerability observed in preclinical studies suggests a safer profile compared to traditional therapies, a critical consideration for young patients. Healthcare providers should collaborate with research bodies to monitor progress and advocate for accelerated trial phases, ensuring that promising outcomes are not delayed in reaching those in need. This proactive stance can bridge the gap between lab and clinic.
Addressing Challenges in Dietary Implementation
One of the primary hurdles in adopting this treatment is the difficulty of enforcing a strict diet in children, which can be logistically and emotionally challenging. Best practice involves developing support systems, including access to nutritionists and behavioral specialists, to assist families in maintaining dietary compliance. Creative solutions, such as child-friendly recipes, can make adherence more feasible.
Additionally, ongoing efforts to develop an enzyme as a substitute for dietary restrictions should be closely followed by medical professionals. Supporting research into this alternative can alleviate practical barriers, making the therapy more accessible. Until such innovations are available, clear communication with families about the importance of the diet remains paramount for treatment success.
Collaborative Efforts and Future Readiness
Fostering International Partnerships for Advancement
Collaboration with global institutions, such as the Children’s Hospital of Philadelphia and Princeton University, is a vital best practice for advancing this treatment. Medical communities should actively engage in these partnerships to share knowledge, resources, and expertise, ensuring a comprehensive approach to clinical development. Such alliances can expedite the path to establishing this method as a standard of care.
Participation in international research networks also allows for diverse perspectives and larger patient cohorts in trials, enhancing the robustness of findings. Clinicians and researchers are encouraged to contribute to these efforts, fostering a collective push toward innovative solutions for neuroblastoma. This collaborative spirit is essential for overcoming complex challenges in pediatric oncology.
Preparing for Clinical Trials and Beyond
As this drug-diet combination moves closer to human trials, best practice dictates that healthcare providers and families stay informed about enrollment opportunities and eligibility criteria. Advocating for patient involvement in these studies can provide critical data while offering access to cutting-edge care. Educational outreach ensures that stakeholders understand the potential impact of their participation.
Moreover, maintaining a balanced perspective on the therapy’s prospects is crucial. While optimism surrounds the preclinical outcomes, acknowledging the need for further validation helps manage expectations and focuses efforts on rigorous testing. Continuous updates on trial progress, especially over the coming years from 2025 onward, will be key to integrating this approach into mainstream treatment options.
Reflecting on Progress and Next Steps
Looking back, the journey of developing this drug-diet combination for neuroblastoma showcased a remarkable blend of innovation and dedication, with preclinical studies revealing a path to slow tumor growth and transform cancer cells into functional nerve cells. The emphasis on gentler, targeted therapies marked a significant departure from the harsh effects of conventional treatments, setting a foundation for hope in pediatric cancer care.
Moving forward, the focus shifts to actionable steps like initiating clinical trials to validate the approach in human patients, ensuring that safety and efficacy remain at the forefront. Encouraging families and healthcare providers to engage with emerging research and trial opportunities becomes a priority, as does supporting the development of alternatives to dietary restrictions. These efforts aim to refine and broaden access to this promising therapy, paving the way for a potential new standard in treating high-risk neuroblastoma.